Large meta-analysis confirms efficacy of statins in primary CVD prevention, but individual benefit-harm profiles vary
Comparative effectiveness and safety of statins as a class and of specific statins for primary prevention of cardiovascular disease: A systematic review, meta-analysis and network meta-analysis of randomized trials with 94,283 participants
Literature - Yebyo HG, Aschmann HE, Kaufmann M et al. - Am Heart J 2019; https://doi.org/10.1016/j.ahj.2018.12.007Introduction and methods
The role of statins for primary prevention of CV events is highly debated [1-4]. Some see great potential for statins to reduce the burden of CVD and they recommend life-long use of statins for many healthy individuals [5-8]. Others argue that the evidence-base and decision support for individuals and health care professionals has not yet been developed enough.
Current guidelines used data obtained from systematic reviews and meta-analyses. However, these studies often suffer from limitations. Several meta-analyses reported effects of statins on composite outcomes only, while statins may have opposite effects for certain outcomes and their effect size on different outcomes may vary substantially [9-11]. Various systematic reviews examined statins as a class, which may conceal differences in efficacy and safety between individual statins [12]. Moreover, some of the systematic reviews mixed primary and secondary prevention populations, even though effects might differ between these groups. Plus, primary prevention populations are often prescribed low-dose statins [3,13,14].
To inform the debate on statins, a comprehensive systematic review, meta-analysis and drug-level network meta-analysis of RCTs was conducted (January 2013 – November 2018) to estimate the effectiveness and safety of statins as a class and of individual statins for primary prevention of CVD. Eligible open-label or double-blind RCTs (40 trials; n=94.283) compared a statin vs. placebo (33 trials) or a statin vs. another statin (7 trials) and reported results on at least one benefit or harm outcome in people without history of any CVD events at baseline (median age: 58.3 years). Six statins were considered: simvastatin, lovastatin, fluvastatin, atorvastatin, pravastatin, and rosuvastatin. Median follow-up was 1 year. Primary outcomes were CVD events or all-cause mortality.
Main results
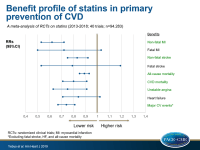
Effects of statins on benefit outcomes
- Risk of non-fatal MI was significantly reduced with statins as a class (RR: 0.62, 95%CI: 0.53-0.72, I²=28.6%), compared to placebo. In the drug-level network analysis, non-fatal MI events were significantly reduced with atorvastatin, rosuvastatin and pravastatin, but not with lovastatin. Most effective treatment was observed with atorvastatin.
- Risk of fatal MI was significantly reduced with atorvastatin, while the other specific statins as well as statins as a class (RR: 0.72, 95%CI: 0.50-1.03, I²=0%) did not show significant effects.
- Statins as a class reduced the risk of non-fatal stroke (RR: 0.83, 95%CI: 0.75-0.92; I²=0). In the drug-level analysis, only the effect of rosuvastatin and atorvastatin were statistically significant.
- Neither statins as a class (RR: 0.79, 95%CI: 0.53-1.19; I²=0), nor individual statins had a significant effect on fatal stroke.
- All-cause mortality was significantly reduced with statins as a class (RR: 0.89, 95%CI: 0.85-0.93, I²=0%), compared with placebo. Individually, pravastatin, atorvastatin, and rosuvastatin showed statistically significant risk reductions of all-cause mortality.
- CVD mortality was significantly reduced with statins as a class (RR: 0.80, 95%CI: 0.71-0.91, I²=35.2%), compared with placebo. However, in drug-level analysis, only the effects of rosuvastatin and pravastatin on CVD mortality were significant.
- Fewer events of unstable angina were observed with statins as a group (RR: 0.75, 95%CI: 0.63-0.91, I²=0%), compared with placebo. However, in drug-level analysis, only the effect of atorvastatin reached statistical significance.
- Neither statins as a class (RR: 0.84, 95%CI: 0.71-1.02, I²=0%) nor individual statins significantly reduced the risk of HF, compared to placebo.
- The composite outcome of all major CV events (excluding fatal stroke, HF, and all-cause mortality) was significantly reduced with statins as a class (RR: 0.74, 95%CI: 0.67-0.81, I²=0%), compared with placebo.
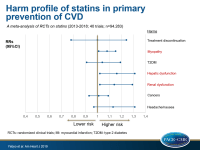
Effects of statins on harm outcomes
- Both relative and absolute risk of myopathy were significantly increased with statins as a class (RR: 1.08, 95%CI: 1.01-1.15, I²=1.15%), compared with placebo. However, none of the statins individually showed a significant effect.
- Statins as a class did not have significant effects on T2DM (RR: 1.04, 95%CI: 0.91-1.19). However, subjects randomized to atorvastatin and rosuvastatin showed more diabetes events, compared with placebo.
- Hepatic dysfunction was increased with statins as a class (RR: 1.16, 95%CI: 1.02-1.31, I²=0%), compared with placebo. In drug-level analysis, fluvastatin reached statistical significance with a five-fold higher risk, compared with placebo.
- Relative risk of renal dysfunction was higher with statins as a class (RR: 1.14, 95%CI: 1.02-1.29, I²=4.6%), compared with placebo. In drug-level analysis, only the effect of rosuvastatin was statistically significant.
- Neither statins as a class, nor individual statins significantly affected treatment discontinuation due to adverse events, cancers, and headache and nausea, compared to placebo.
Conclusion
This systematic review, meta-analysis and network meta-analysis of RCTs on statins demonstrated efficacy both of statins as a class and of specific statins in prevention of CV events and all-cause mortality in primary prevention populations. However, increased risk of myopathy, renal dysfunction and hepatic dysfunction were observed. The benefit-harm profiles differed among individual statins. Atorvastatin and rosuvastatin appeared to be the most effective and atorvastatin the safest statin across most of the outcomes.
References
1. Cholesterol Treatment Trialists. Efficacy and safety of more intensive lowering of LDL cholesterol : a meta-analysis of data from 170 000 participants in 26 randomised trials. Lancet 2010;376:1670–81.
2. Otto CM. Statins for primary prevention of cardiovascular Patients need better tools to navigate divergent recommendations. BMJ 2016;355:1–2.
3. Cholesterol Treatment Trialists. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease : meta-analysis of individual data from 27 randomised trials. Lancet 2012;380:581–90.
4. Naci H, Brugts J, Ades T. Comparative tolerability and harms of individual statins : A study-level network meta-analysis of 246 955 participants from 135 randomized, controlled trials. Circ Cardiovasc Qual Outcomes 2013;6:390–9.
5. US Preventive Services Tast Force. Statin Use for the Primary Prevention of Cardiovascular. JAMA 2016;316:1997–2007.
6. Stone N, Robinson J, Lichtenstein A, et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Can J Hosp Pharm 2014;67:246–7.
7. Catapano AL, Chairperson IG, France MJC, et al. 2016 ESC / EAS Guidelines for the Management of Dyslipidaemias The Task Force for the Management of Dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS) Developed with the special contribution of the Eu. Atherosclerosis 2016;253:281–344.
8. Stone NJ, Robinson JG, Lichtenstein AH, et al. ACC / AHA Prevention Guideline 2013 ACC / AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults A Report of the American College of Cardiology / American Heart Association Task Force on Practice Guidel. C
9. Collins R, Reith C, Emberson J, et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet 2016; 388:2532–61.
10. Pogue J, Devereaux PJ, Thabane L, et al. Designing and Analyzing Clinical Trials with Composite Outcomes : Consideration of Possible Treatment Differences between the Individual Outcomes. PLoS One 2012;7:e34785.
11. Prieto-merino D, Smeeth L, Staa TP Van, et al. Dangers of non-specific composite outcome measures the effect of treatment. BMJ 2013;6782:1–6. irculation 2014;129:Suppl 1-50.
12. Chou R, Dana T, Daeges M, et al. Statins for Prevention of Cardiovascular Disease in Adults Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2016;316:2008–24.
13. Redberg RF, Katz MH. Statins for primary prevention: The debate is intense, but the data are weak. JAMA 2016;316:1979–81.
14. Collins R, Reith C, Emberson J, et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet 2016;388:2532–61.

Facebook Comments