Elevated pro-inflammatory biomarkers associated with decompensation in HFpEF
Levels of pro-inflammatory biomarkers were significantly elevated in decompensated compared with stable HF patients with preserved ejection fraction, and some were linked with altered diastolic function.
Pro‐Inflammatory Biomarkers in Stable Versus Acutely Decompensated Heart Failure With Preserved Ejection FractionLiterature - Abernethy A, Raza S, Sun J-L, et al. - J Am Heart Assoc. 2018;7:e007385
Introduction and methods
Elevations in blood levels of pro-inflammatory biomarkers have been associated with severity and prognosis of heart failure with reduced ejection fraction (HFrEF), but it is not known whether this also true for heart failure with preserved ejection fraction (HFpEF) [1].
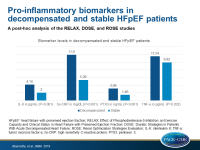
This post-hoc analysis of three studies assessed whether selected pro-inflammatory biomarkers are elevated in patients with acute decompensated (AD) HFpEF compared with patients with stable (S) HFpEF. Moreover it evaluated whether biomarker levels are associated with echocardiographic-Doppler abnormalities of left ventricular diastolic function, and whether they are predictive of clinical outcomes in AD-HFpEF patients. Clinical outcomes included urine volume, change in cystatin-C, change in creatinine, change in NT-proBNP, and change in weight over the 72 hours after randomization, as well as post-discharge survival and re-hospitalizations at 60 days.
For this purpose, interleukin 6 (IL-6), tumor necrosis factor-α (TNF-α), high sensitivity C-reactive protein (hs-CRP) and pentraxin 3 (PTX3) levels were measured in age and sex-matched cohorts of HFpEF patients from 3 prospective, placebo-controlled, randomized clinical trials:
- RELAX (Effect of Phosphodiesterase-5 Inhibition on Exercise Capacity and Clinical Status in Heart Failure with Preserved Ejection Fraction), with S-HFpEF patients [2]
- DOSE (Diuretic Strategies in Patients With Acute Decompensated Heart Failure) [3]
- ROSE (Renal Optimization Strategies Evaluation) [4]
DOSE and ROSE included AD patients with HFrEF and HFpEF.
Main results
- Compared with the S-HFpEF group, the AD-HFpEF cohort had significantly higher levels of IL-6 (4.14 pg/mL vs 2.00 pg/mL; P<0.001), hs-CRP (11.90 mg/dL vs. 5.36 mg/dL; P<0.001) and PTX3 (3.08 ng/mL vs 1.46 ng/mL; P<0.001), but there was no statistically significant difference in TNF-α (11.54 pg/mL vs 9.92 pg/mL; P=0.202).
- PTX3 was positively correlated with left atrial volume index (P=0.002; r=0.41) and left ventricular mass (P=0.042; r=0.26), while elevated TNF-α was found to be inversely correlated with the E/A ratio for diastolic function (P=0.040; r=-0.31). IL-6 and hs-CRP were not significantly correlated with any measures of diastolic function.
- There were no statistically significant associations between urine volume, change in cystatin-C, change in creatinine, change in NT-proBNP, or change in weight and biomarker levels.
- None of the biomarkers were significantly associated with re-admission or death. After adjustment for age, IL-6 was statistically significant associated with 60 day death or heart failure re-hospitalization (HR: 1.097; 95%CI: 1.003–1.201; P=0.043).
Conclusion
Levels of three pro-inflammatory biomarkers were significantly elevated in decompensated patients with HFpEF compared with stable HFpEF patients. These results suggest that chronic inflammation plays a role in the pathophysiology of HFpEF and that inflammatory marker levels increase during decompensation. This may provide a rationale for targeted anti-inflammatory therapy in HFpEF.
References
1. Levine B, Kalman J, Mayer L, et al. Elevated circulating levels of tumor necrosis factor in severe chronic heart failure. N Engl J Med.1990;323:236–241.
2. Redfield MM, Chen HH, Borlaug BA, et al. Effect of phosphodiesterase-5 inhibition on exercise capacity and clinical status in heart failure with preserved ejection fraction: a randomized clinical trial. JAMA. 2013;309:1268–1277.
3. Felker GM, Lee KL, Bull DA, et al. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 2011;364:797–805.
4. Chen HH, Anstrom KJ, Givertz MM, et al. Low-dose dopamine or low-dose nesiritide in acute heart failure with renal dysfunction: the ROSE acute heart failure randomized trial. JAMA. 2013;310:2533–2543.