HDL-C and residual cardiovascular risk in relation to lipid-lowering medication
HDL-C levels are not related to vascular risk in patients using intensive lipid-lowering medication.
Low HDL-cholesterol is not a risk factor for recurrent vascular events in patients with vascular disease on intensive lipid-lowering medicationLiterature - Van de Woestijne et al. JACC 2013 - JACC 2013
Van de Woestijne AP, van der Graaf Y, Liem AH, et al.
J Am Coll Cardiol. 2013;62:1834-41
Background
Low levels of high-density lipoprotein-cholesterol (HDL-C) are an important risk factor for vascular disease, both in healthy populations [1–3] and in patients with known vascular disease [4–6]. Although these patients are already intensively treated for risk factors such as high levels of low-density lipoprotein-cholesterol (LDL-C), they are still at a high residual risk for vascular events. Low HDL-C is a risk factor for vascular disease independent of LDL-C [7], even when LDL-C is at target level, and this is still apparent in patients with vascular disease [4,6,8].Statin trials in patients with coronary artery disease have seen a lack of the inverse relation between HDL-C and risk of vascular events in patients receiving (intensive) statin therapy [9,10,11], albeit with a fixed statin dose, whereas according to current guidelines, LDL-C is treated to target, with various dosages of different statins including combination therapy. As many patients with clinically manifest vascular disease are treated with statins, the residual risk from HDL-C in these patients may be smaller than initially thought.
This study evaluated the vascular risk of low HDL-C in relation to the use and intensity of lipid-lowering medication in patients with clinically manifest vascular diseases. A prospective cohort study was performed in 6,111 patients with manifest vascular disease. Cox proportional hazards models were used to evaluate the risk of HDL-C on vascular events in patients using no, usual dose, or
intensive lipid-lowering therapy.
Main results
- New vascular events (myocardial infarction, stroke, or vascular death) occurred in 874 subjects during a median follow-up of 5.4 years (interquartile range: 2.9 to 8.6 years).
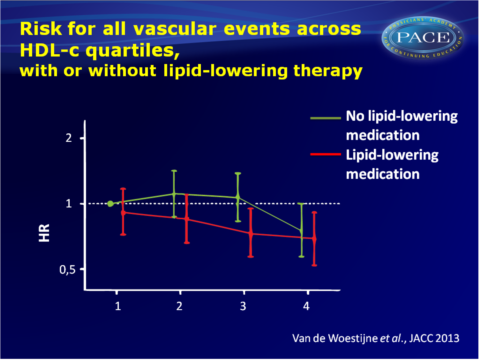
- In patients not using lipid-lowering medication at baseline (n = 2,153), a 0.1 mmol/l increase in HDL-C was associated with a 5% reduced risk for all vascular events (hazard ratio [HR]: 0.95; 95% confidence interval [CI]: 0.92 to 0.99).
- In patients on usual dose lipid-lowering medication (n = 1,910) there was a 6% reduced risk (HR: 0.94; 95% CI: 0.90 to 0.98).
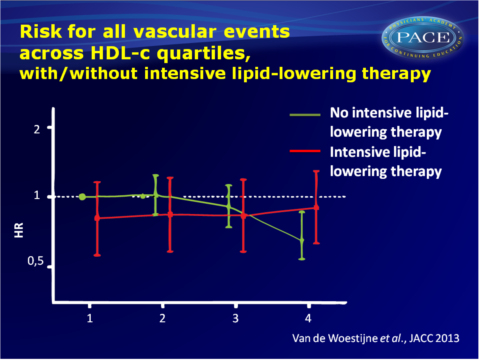
- However, in patients using intensive lipid-lowering treatment (n = 2,046), HDL-C was not associated with recurrent vascular events (HR: 1.02; 95% CI: 0.98 to 1.07) irrespective of LDL-C level.
- In quartiles of higher HDL-C, the risk of vascular events was lower in patients on usual dose lipid-lowering therapy compared with the lowest HDL-C quartile.
- For patients on intensive lipid-lowering therapy, the overall risk for vascular events was lower compared with patients using no or usual dose lipid-lowering, but there was no relation between HDL-C and vascular risk in that group.
Download Vd Woestijne_SMART_pace.pptx
Conclusion
HDL-C levels are related to the risk of new cardiovascular events in patients with clinically manifest vascular disease treated with usual dose lipid-lowering therapy but not in patients treated with intensive lipid-lowering medication, irrespective of LDL-C.Editorial comment [12]
This study suggests that the measurement of HDL-C in patients with established atherosclerotic cardiovascular disease treated with intensive LDL-C lowering no longer predicts future cardiovascular events. The “HDL hypothesis” states that raising HDL-C prevents cardiovascular disease, but this has been severely challenged of late. Current guidelines for the prevention and treatment of cardiovascular disease should continue to focus on LDL-C as the major therapeutic target. Non–HDL-C (i.e., the sum of apo B-containing lipoproteins) or apo B itself are solid therapeutic targets as well. There is little support from clinical trials to attempt to raise HDL-C pharmacologically. To date, the trial evidence is at best neutral; at worst, there is evidence of harm. The link of causality between HDL-C and cardiovascular disease might have to be rethought . Better biomarkers of HDL function have to be developed and tested in clinical trials.For the time being, the concept of HDL-C as representing an important proportion of residual cardiovascular risk in patients on appropriate statin dosage is not well supported by data.
Find this article online
References
1. Castelli WP, Garrison RJ, Wilson PW, et al. Incidence of coronary heart disease and lipoprotein cholesterol levels. The Framingham Study. JAMA 1986;256:2835–8.
2. Sharrett AR, Ballantyne CM, Coady SA, et al. Coronary heart disease prediction from lipoprotein cholesterol levels, triglycerides, lipoprotein (a), apolipoproteins A-I and B, and HDL density subfractions-The Atherosclerosis Risk in Communities (ARIC) Study. Circulation 2001;104:1108–13.
3. Di Angelantonio E, Sarwar N, Perry P, et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA 2009;302:1993–2000.
4. Hajer GR, van der Graaf Y, Bots ML, et al. Low plasma HDL-c, a vascular risk factor in high risk patients independent of LDL-c. Eur J Clin Invest 2009;39:680–8.
5. Pekkanen J, Linn S, Heiss G, et al. Ten-year mortality from cardiovascular disease in relation to cholesterol level among men with and without preexisting cardiovascular disease. N Engl J Med 1990;322:1700–7.
6. Sacks FM, Tonkin AM, Craven T, et al. Coronary heart disease in patients with low LDL-cholesterol: benefit of pravastatin in diabetics and enhanced role for HDL-cholesterol and triglycerides as risk factors. Circulation 2002;105:1424–8.
7. Fruchart JC, Sacks F, Hermans MP, et al. The Residual Risk Reduction Initiative: a call to action to reduce residual vascular risk in patients with dyslipidemia. Am J Cardiol 2008;102:1–34K.
8. Seo SM, Choo EH, Koh YS, et al. High-density lipoprotein cholesterol as a predictor of clinical outcomes in patients achieving lowdensity lipoprotein cholesterol targets with statins after percutaneous coronary intervention. Heart 2011;97:1943–50.
9. Ridker PM, Genest J, Boekholdt SM, et al. HDL cholesterol and residual risk of first cardiovascular events after treatment with potent statin therapy: an analysis from the JUPITER trial. Lancet 2010;376: 333–9.
10. Sacks FM, Moye LA, Davis BR, et al. Relationship between plasma LDL concentrations during treatment with pravastatin and recurrent coronary events in the Cholesterol and Recurrent Events trial. Circulation 1998;97:1446–52.
11. Ray KK, Cannon CP, Cairns R, Morrow DA, Ridker PM, Braunwald E. Prognostic utility of apoB/AI, total cholesterol/HDL, non-HDL cholesterol, or hs-CRP as predictors of clinical risk in patients receiving statin therapy after acute coronary syndromes: results from PROVE IT-TIMI 22. Arterioscler Thromb Vasc Biol 2009;29:424–30.
12. Genest J. HDL and Residual Cardiovascular Risk: De minimis non curat medicus? Or: The COURAGE to be SMART.
J Am Coll Cardiol. 2013;62:1842-44
