Guideline differences regarding statin treatment affect ASCVD event prevention
Statin eligibility differs substantially in the 5 major guidelines, and this impacts on the potential prevention of ASCVD events, which is a function of the number of eligible persons for statin therapy.
Comparison of Five Major Guidelines for Statin Use in Primary Prevention in a Contemporary General PopulationLiterature - Mortensen MB and Nordestgaard BG. - Ann Intern Med 2018;168(2):85-92
Background
Statin therapy is very important for the prevention of atherosclerotic cardiovascular disease (ASCVD), and currently, there are 5 major published guidelines with recommendations on how to use them:
- the ACC/AHA guidelines: American College of Cardiology/American Heart Association [1]
- the NICE guidelines: UK National Institute for Health and Care Excellence [2]
- the CCS guidelines: Canadian Cardiovascular Society [3]
- the USPSTF guidelines: U.S. Preventive Services Task Force [4]
- the ESC/EAS guidelines: European Society of Cardiology/European Atherosclerosis Society [5]
Although all guidelines are based on the same evidence, they differ significantly in their recommendations. The impact of these differences in clinical practice is not known. This study evaluated the clinical performance of the 5 major statin therapy guidelines in 45,750 participants of the Copenhagen General Population Study (CGPS), an ongoing prospective cohort study of the Danish general population [6].
Eligible participants were 40-75 years old, had no ASCVD, were not on statins at baseline, and had a minimum of 5 years of follow-up. The potential effect of each guideline on ASCVD prevention in the general population during 10 years of follow-up, was assessed either with high-intensity statins (assuming a 50% LDL-c reduction) or with moderate-intensity statins (assuming a 30% LDL-c reduction), with a given 25% reduction in ASCVD events per 1 mmol/L (38.7 mg/dL) LDL-c reduction. ASCVD events were defined as non-fatal MI, fatal CHD, and stroke.
Main results
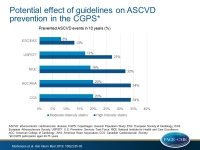
- Statin eligibility was determined for 44% of participants according to CCS, 42% according to ACC/AHA, 40% according to NICE, 31% according to USPSTF, and 15% according to ESC/EAS guidelines.
- There was a relative 59%-76% agreement in statin eligibility among the CCS, ACC/AHA, NICE, and USPSTF guidelines but only 25%-31% agreement between ESC/EAS and other guidelines.
- The potential event reduction of each guideline for the duration of 10 years was 34% for CCS, 34% for ACC/AHA, 32% for NICE,27% for USPSTF, and 13% for ESC/EAS with high-intensity statin therapy, and 20%, 20%, 19%, 17%, and 8%, respectively for moderate-intensity statins.
- In general, the more persons were eligible for statin therapy in primary prevention based on guidelines, the more ASCVD events could have been prevented.
- In a sensitivity analysis including class IIa recommendations (ACC/AHA and ESC/EAS), and grade C recommendations (USPSTF guidelines), statin eligibility increased to 53% (up by 11%) of the population with the ACC/AHA guideline, 38% (up by 7%) with the USPSTF guideline, and 18% (up by 3%) with the ESC/EAS guideline. This corresponded with increased potential ASCVD event reduction: 38% (up by 4%) for ACC/AHA, 31% (up by 4%) for USPSTF, and 15% (up by 2%) for the ESC/EAS guideline.
Conclusion
Statin eligibility differs substantially in the 5 major guidelines, and this impacts on the potential prevention of ASCVD events, which is a function of the number of eligible persons for statin therapy. Assuming negligible harm and low costs of statin therapy, the authors recommend to use the ACC/AHA or the CCS guidelines, rather than the ESC/EAS or USPSTF guidelines, in order to prevent more ASCVD events.
Editorial comment
In his editorial article [7], Mancini notes the complexity of developing medical guidelines and notes that differences in recommendations ‘….reflect the priorities, preferences, local needs, and practical realities of intended users.’ He mentions the limitations of the Mortensen et al study, which include the use of ASCVD end points other than those in the guidelines, the modeling of relative LDL-c reductions only, and the lack of examination of potential harm and cost of therapy, and he concludes: ‘Thus, although each organization must continue to evaluate the science in a fashion relevant to their priorities and the realities (including economics) of the settings in which their clinicians practice, Mortensen and Nordestgaard highlight how approaches liberalizing statin use for primary prevention and emphasizing large LDL-C reductions are expected to achieve greater reduction in ASCVD. They motivate us to examine whether the risk algorithms should be replaced by more sophisticated risk calculators or by the simpler approaches of randomized trials.’
References
1. Stone NJ, Robinson JG, Lichtenstein AH, et al; American College of Cardiology/American Heart
Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2889-934.
2. National Institute for Health and Care Excellence. Lipid Modification: Cardiovascular Risk Assessment and the Modification of Blood Lipids for the Primary and Secondary Prevention of Cardiovascular Disease. Clinical Guideline CG181. London: National Clinical Guideline Centre; July 2014.
3. Anderson TJ, Gre´goire J, Pearson GJ, et al. 2016 Canadian Cardiovascular Society guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol. 2016;32:1263-82.
4. Bibbins-Domingo K, Grossman DC, Curry SJ, et al; US Preventive Services Task Force. Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force recommendation statement. JAMA. 2016;316:1997-2007.
5. Piepoli MF, Hoes AW, Agewall S, et al; Authors/Task Force Members. 2016 European guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37:2315-81.
6. Mortensen MB, Nordestgaard BG, Afzal S, et al. ACC/AHA guidelines superior to ESC/EAS guidelines for primary prevention with statins in non-diabetic Europeans: the Copenhagen General Population Study. Eur Heart J. 2017;38:586-94.
7. Mancini JGB. Comparison Shopping: Guidelines for Statins for Primary Prevention of Cardiovascular Disease. Ann Intern Med. 2018;168:145-146.