Post-ACS patients do not benefit from addition of a NOAC to DAPT
Meta-analysis shows that in patients with recent ACS, addition of a NOAC to dual antiplatelet therapy resulted in a modest reduction of major adverse CV events but led to higher bleeding risk.
Meta-Analysis of the Safety and Efficacy of the Oral Anticoagulant Agents (Apixaban, Rivaroxaban, Dabigatran) in Patients With Acute Coronary SyndromeLiterature - Khan SU, Arshad A, Riaz IB, et al. - Am J Cardiol 2018;121:301–307
Background
Patients with acute coronary syndromes (ACS) are at risk of suffering recurrent major adverse cardiovascular events (MACE), particularly during the first few months post-ACS, even if they receive optimal dual antiplatelet therapy (DAPT) [1-3]. The new oral anticoagulants (NOACs) are effective and safe as stroke prophylaxis in non-valvular atrial fibrillation, but their antithrombotic potential after an ACS is less clear [4,5].
In this meta-analysis, the relative safety and efficacy of the NOACs rivaroxaban, apixaban, and dabigatran was evaluated, when added to single antiplatelet agent (SAP) or DAPT, in patients with a recent ACS. Seven randomized clinical trials reporting outcomes of interest (clinically significant bleeding and MACE) in adults with ACS met inclusion criteria : APPRAISE, APPRAISE-2, ATLAS ACS-TIMI 46, ATLAS ACS-TIMI 51, REDEEM, PIONEER AF and RE DUAL PCI. Patients on NOAC dosages causing a very high bleeding risk were excluded from the analysis, leaving:
- 70% of patients from APPRAISE (total N=1,210; apixaban vs placebo)
- 99% of patients from APPRAISE 2 (total N=7,315; apixaban vs placebo)
- 57% of patients from ATLAS ACS-TIMI 46 (total N=1,997; rivaroxaban vs placebo)
- 98% of patients from ATLAS ACS-TIMI 51 (total N=15,342; rivaroxaban vs placebo)
- 100% of patients from PIONEER AF (total N=2,124; rivaroxaban vs warfarin)
- 99% of patients from REDEEM (total N=1,861; dabigatran vs placebo)
The RE DUAL PCI (total N=1,743; dabigatran vs warfarin) enrolled only 50% patients with ACS, and was excluded from the secondary efficacy outcome as the study defined MACE differently. For this analysis, the International Society of Thrombosis and Hemostasis (ISTH) bleeding criteria were selected, and the Thrombolysis in Myocardial Infarction (TIMI) criteria were used only if ISTH criteria were not available.
Main results
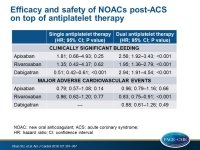
- In 31,574 patients, addition of a NOAC to SAP did not increase the risk of clinically significant bleeding (HR: 0.82; 95%CI: 0.56-1.20; P=0.31), and had no beneficial efficacy effect on MACE (HR: 0.82; 95%CI: 0.66-1.04; P=0.10).
- A modest reduction in MACE was achieved when a NOAC was combined with DAPT (HR: 0.86; 95%CI: 0.78- 0.93; P<0.001), which was accompanied by a more than doubled risk of bleeding (HR: 2.24; 95%CI: 1.75-2.87; P<0.001).
- In subgroup analyses that assessed the effects of individual NOACs, dabigatran plus SAP was a safer approach compared with control (HR: 0.51; 95%CI: 0.42-0.61; P<0.001), and only rivaroxaban plus DAPT showed a significant 17% reduction in MACE. All the individual NOACs increased bleeding risk significantly when added to DAPT without achieving a meaningful MACE benefit.
Conclusion
In patients with recent ACS, addition of NOAC to single antiplatelet therapy did not result in excessive bleeding events or reduction in MACE. Addition of NOAC to dual antiplatelet therapy did result in a modest MACE reduction but led to an increased bleeding risk. Among NOACs, only rivaroxaban plus DAPT reduced the risk of MACE, and dabigatran plus SAP was the safest approach.
References
1. Paravattil B, Elewa H. Strategies to optimize dual antiplatelet therapy after coronary artery stenting in acute coronary syndrome. J Cardiovasc Pharmacol Ther 2017;22:347–355.
2. Libby P. Mechanisms of acute coronary syndromes. N Engl J Med 2013;369:883–884.
3. Monroe DM, Hoffman M, Roberts HR. Platelets and thrombin generation. Arterioscler Thromb Vasc Biol 2002;22:1381–1389.
4. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009;361:1139–1151.
5. Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 2011;365:883–891.