PCSK9 variants have no effect on the risk of stroke
//PCSK9// genetic variants, that produce lower levels of LDL-c, are not associated with the risk of ischemic stroke, in contrast to significant association with the risk of CHD.
Differential effects of PCSK9 variants on risk of coronary disease and ischaemic strokeLiterature - Hopewell JC, et al. - Eur Heart J 2018;39:354–359
Background
Low-density lipoprotein cholesterol (LDL-c) levels have been associated with coronary heart disease (CHD) and with ischemic stroke (IS), but the latter relationship is not well established [1]. PCSK9 variants are useful to study the strength of association between LDL-c and IS.I
n this study, the association of PCSK9 genetic variants with IS risk was evaluated, in more than 10,000 well-characterized IS cases, and the strength of association was compared with that of CHD risk. For this purpose, the following PCSK9 genetic variants were selected:
- the rare loss-of-function (LOF) missense rs11591147 (R46L) polymorphism, which has a large effect on PCSK9 and LDL-c levels, and is strongly associated with CHD [2]
- the common missense variants rs562556 [V474I], rs505151[E670G], and rs11583680 [A53V]
- the common non-coding variants rs11206510 and rs2479409
The effects of each variant on risk were examined separately and a weighted genetic risk score was constructed including only the two independent variants rs11591147 and rs505151.
Data from 3 genome-wide meta-analyses were used, which included 10,307 IS cases and 19,326 controls of European ancestry: the Global Lipids Genetics Consortium (GLGC) [10], the CARDIoGRAMPlusC4D Consortium [12], the METASTROKE Collaboration [13].
Main results
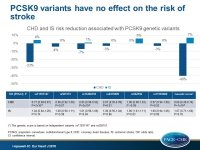
- The low frequency (1.5%) rs11591147 (R46L) LOF variant was associated with a 0.5 mmol/L (95%CI: 0.47–0.54; P=9x10-143) lower LDL-c level per T allele.
- rs11591147 (R46L) LOF variant was associated with a 23% lower risk of CHD (OR: 0.77; 95%CI: 0.69–0.87; P=7x10-6), but it was not associated with IS risk (OR: 1.04; 95%CI: 0.84–1.28; P=0.74), and there was no significant heterogeneity of the effect on IS between the contributing studies (P=0.26).
- Overall, the association of rs11591147 (R46L) with IS risk was significantly different to that with CHD risk (P for heterogeneity = 0.02).
- The five additional PCSK9 variants ranged in frequency from 14.1% to 96.5% for the LDL-lowering allele. Each of the additional PCSK9 variants was significantly associated with LDL-c levels, with effects ranging from 0.09 mmol/L lower LDL-c per allele (95%CI: 0.07–0.11; P=4x10-17) for rs505151 to 0.03 mmol/L lower LDL-c per allele (95%CI: 0.02–0.05; P=1x10-8) for rs11583680.
- There were no apparent associations of any of the other PCSK9 variants with IS risk, and no significant heterogeneity between the effects of all six variants on IS risk when scaled to the same LDL-c difference (P=0.56).
- There were also no significant associations of rs11591147 (R46L) or any of the other PCSK9 variants with cardioembolic, large artery or small vessel disease stroke.
- The PCSK9 genetic risk score was associated with a 40% lower risk of CHD (OR: 0.60; 95%CI: 0.49–0.74; P=1x10-6) and a non-significant effect on IS (OR: 1.07; 95%CI: 0.71–1.60; P=0.76) per 1 mmol/L lower LDL-c, suggesting significant heterogeneity between the effects of PCSK9 on CHD and on IS risk (P for heterogeneity = 0.01).
Conclusion
//PCSK9// genetic variants, that produce lower levels of LDL-c, are not associated with the risk of IS, in contrast to significant association with the risk of CHD.
Editorial comment
In his editorial article, Ference [6] focuses on the Mendelian randomization methodology, rather than the findings of the study published by Hopewell et al. He analyzes the limitations of the analogy of the so-called ‘nature’s randomized trials’ (Mendelian randomized study) and a randomized trial that include the translation of causal effect of lifelong changes in an exposure on an outcome to the expected effect in response to short-term therapeutically induced changes in that exposure on the outcome. He includes as well the danger of overestimating the expected effect size, when using Mendelian randomization outcomes to foresee the results of a randomized trial. The author concludes: ‘Mendelian randomization studies can be used to anticipate the results of randomized trials accurately. However, a common misconception is that a therapy directed against any causal exposure will probably improve the associated outcome. Unfortunately, finding that an exposure is causally associated with an outcome tells us almost nothing about whether a therapy directed against that exposure will improve the outcome in a randomized trial. To anticipate the results of a randomized trial, the critical question that must be answered is by how much the causal exposure must be changed to improve the associated outcome in a short-term randomized trial.’
References
1. The Cholesterol Treatment Trialists’ (CTT) Collaboration. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 2010;376:1670–1681.
2. Cohen JC, Boerwinkle E, Mosley TH Jr, et al. Sequence variations in PCSK9, low LDL, and protection against coronary heart disease. N Engl J Med 2006;354:1264–1272.
3. The Global Lipids Genetics Consortium. Discovery and refinement of loci associated with lipid levels. Nat Genet 2013;45:1274–1283.
4. The CARDIoGRAMplusC4D Consortium. A comprehensive 1000 Genomes based genome-wide association meta-analysis of coronary artery disease. Nat Genet 2015;47:1121–1130.
5. Malik R, Traylor M, Pulit SL, et al. Low-frequency and common genetic variation in ischemic stroke: the METASTROKE collaboration. Neurology 2016;86:1217–1226.
6. Ference BA. How to use Mendelian randomization to anticipate the results of randomized trials. European Heart Journal (2018) 39, 360–362.