Catheter ablation improves mortality and morbidity in patients with heart failure and atrial fibrillation
Catheter ablation is associated with a lower mortality and morbidity rate compared to medical therapy in patients with heart failure and atrial fibrillation.
Catheter Ablation for Atrial Fibrillation with Heart FailureLiterature - Marrouche NF, Brachmann J, Andresen D, et al. - N Engl J Med 2018;378:417-27
Background
The treatment of atrial fibrillation (AF) improves long-term outcomes in patients with heart failure (HF), but the most beneficial treatment option is debated [1]. Catheter ablation is indicated for symptomatic, drug-resistant AF, and some data have shown that it is also associated with positive outcomes in HF patients [2-4].
In the Catheter Ablation versus Standard Conventional Therapy in Patients with Left Ventricular Dysfunction and Atrial Fibrillation (CASTLE-AF) trial, a multicenter, open-label, randomized, controlled trial, the effect of catheter ablation on morbidity and mortality was evaluated compared with medical therapy in HF patients with symptomatic AF.
The main inclusion criteria were: New York Heart Association (NYHA) class II-IV, left ventricular ejection fraction (LVEF) ≤ 35%, paroxysmal or persistent AF not responding to antiarrhythmic drugs, or with serious adverse events due to antiarrhythmic drug therapy, implantation of a Biotronik-manufactured cardioverter–defibrillator (ICD) device or a cardiac resynchronization therapy defibrillator (CRT-D) with automatic daily remote-monitoring capabilities. Patients were randomly assigned in a 1:1 ratio to receive catheter ablation or medical therapy for AF. Medical therapy for AF was administered based on medical guidelines. For all patients, the Biotronik Home Monitoring option was activated to monitor the recurrence of AF. If AF recurred, a repeat ablation was recommended unless contraindicated clinically.
The primary end point was a composite of all-cause death or HF worsening leading to an unplanned overnight hospitalization. Secondary end points included all-cause death, unplanned hospitalization due to HF, death from CVD, LVEF increase and achievement of sinus rhythm.
Main results
- 363 patients met the inclusion criteria and were followed-up for a mean duration of 37.6±20.4 months in the ablation group (179 patients) and 37.4±17.7 months in the medical therapy group (184 patients).
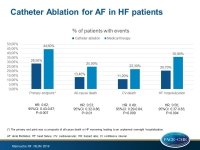
- The composite primary end point occurred in significantly fewer patients in the ablation group compared with the medical-therapy group (28.5% vs. 44.6%; HR: 0.62; 95%CI: 0.43-0.87; P=0.007).
- Rates of all-cause death were 13.4% in the ablation group and 25.0% in the medical-therapy group (HR: 0.53; 95%CI: 0.32-0.86; P=0.01).
- Rates of HF hospitalizations were 20.7% in the ablation group and 35.9% in the medical-therapy group (HR: 0.56; 95%CI: 0.37-0.83; P=0.004).
- Rates of CV deaths were 11.2% in the ablation group and 22.3% in the medical-therapy group (HR: 0.49; 95%CI: 0.29-0.84; P=0.009).
- The median absolute increase in LVEF was 8.0% (IQ: 2.2-19.1) in the ablation group and 0.2% (IQ: −3.0 to 16.1) in the medical-therapy group (P=0.005). Sinus rhythm was achieved in 63.1% of the patients in the ablation group and in 21.7% of patients in the medical-therapy group (P<0.001).
Conclusion
Catheter ablation is associated with a lower mortality and morbidity rate compared to medical therapy in patients with HF and AF. Moreover, catheter ablation improved the LVEF and reduced the burden of AF.
References
1. Roy D, Talajic M, Nattel SN, et al. Rhythm control versus rate control for atrial fibrillation and heart failure. N Engl J Med 2008; 358: 2667-77.
2. Wazni OM, Marrouche NF, Martin DO, et al. Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of symptomatic atrial fibrillation: a randomized trial. JAMA 2005; 293: 2634-40.
3. Morillo CA, Verma A, Connolly SJ, et al. Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of paroxysmal AF (RAAFT-2): a randomized trial. JAMA 2014; 311: 692-700.
4. Cosedis Nielsen J, Mortensen LS, Hansen PS. Radiofrequency ablation as initial therapy in paroxysmal AF. N Engl J Med 2013; 368: 478-9.