Diabetes increases mortality and morbidity risk in older ischemic stroke patients
In patients with ischemic stroke ≥ 65 years, diabetes is associated with a higher risk of mortality, recurrent events, HF and hospitalisations.
Diabetes and long-term outcomes of ischaemic stroke: findings from Get With The Guidelines-StrokeLiterature - Echouffo-Tcheugui JB, Xu H, Matsouaka RA, et al. - Eur Heart J 2018; published online ahead of print
Background
Diabetic patients have an increased risk of ischemic stroke (IS) compared with non-diabetic individuals, but it is not clear to what extent diabetes mellitus (DM) influences the long-term outcomes after IS [1,2]. In this study, the long-term outcomes of IS patients with and without DM were evaluated.
The data source used was the Get With The Guidelines (GWTG)-Stroke, a US national prospective stroke registry and quality improvement program [3,4]. Patients were eligible for this analysis if they had a diagnosis of IS and were aged ≥65 years. The outcomes were assessed at 1 year and at 3 years post-discharge.
The primary outcome was all-cause mortality. The secondary outcomes included a composite of mortality and all-cause readmission, a composite of death and CV readmission, all-cause admission, admission for recurrent IS or transient ischemic attack (TIA), admission for recurrent IS only, admission for acute myocardial infarction (AMI), admission for heart failure (HF), CV readmission, non-CV admission, and non IS/TIA readmission.
Main results
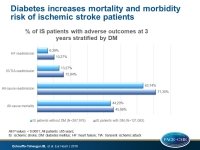
The study sample included 409,060 IS patients from 1,690 sites, out of whom 29.6% had DM. After multivariable adjustment, compared with the non-DM group, DM was associated with higher risks of outcomes. For example, cumulative incidence rates (diabetes vs. no diabetes) and the adjusted hazard ratios at 3 years were:
- all-cause mortality: 45.98% vs. 44.20%, 1.24; 95%CI: 1.23–1.25
- all-cause readmission: 71.30% vs. 63.74%, 1.22; 95%CI: 1.21–1.23
- composite of mortality and all-cause readmission: 84.12% vs. 79.28%, 1.21; 95%CI: 1.20–1.22
- composite of death and CV readmission: 69.45% vs. 64.30%, 1.19; 95%CI: 1.18–1.20
- IS/TIA readmission: 15.94% vs. 13.27%, 1.18; 95%CI: 1.16–1.20
- IS readmission: 12.57% vs. 10.29%, 1.20; 95%CI: 1.18–1.23
- AMI readmission: 4.72% vs. 2.95%, 1.55; 95%CI: 1.49–1.60
- HF readmission: 10.27% vs. 6.39%, 1.60; 95%CI: 1.56–1.64
- non-CV readmission: 58.30% vs. 50.33%, 1.28; 1.26–1.29
- non-IS/TIA readmission: 67.72% vs. 59.72%, 1.23; 95%CI: 1.22–1.25
All P values were <0.0001.
Conclusion
IS patients with diabetes aged ≥65 years are at higher risk of mortality, IS/TIA recurrent events, and hospitalisations compared with IS patients without diabetes. These results support the need for early detection and improved care of IS patients with diabetes.
Editorial comment
In their editorial article, Fadini and Cosentino [5] highlight the strengths and weaknesses of the study by Echouffo-Tcheugoui et al. Strengths include the large sample size, the prospective methodology, the sole selection of the ischemic stroke subtype, and the robust adjustment for clinical characteristics, whereas the weaknesses include the exclusion of patients younger than 65 years, an indirect case-related database linkage, and the possibility of residual confounders. Furthermore, they discuss what could drive the poor outcome of IS patients with diabetes and summarize the results of trials with new glucose-lowering drugs that have an impact on CV outcomes, and more specifically on stroke. Overall, the authors recognize the need to improve the care of diabetic patients after ischemic stroke and they conclude: ‘Nowadays, new preventive, diagnostic, and therapeutic opportunities are emerging to improve the care of diabetic patients after ischaemic stroke. However, paradoxically, the use of SGLT2 inhibitors to prevent hospitalisation for heart failure (HHF) in type 2 diabetes is not lowering stroke risk but may even increase it, whereas glucose-lowering medications with potential benefits on stroke risk exert no protection against HHF (GLP-1RA) or may increase HHF risk (pioglitazone). These striking examples of competing cardiovascular outcomes in patients with diabetes suggest that randomized controlled trials should look beyond simplistic composite endpoints and, especially, explore combination therapies that may be particularly effective. Comprehensive management of CVD in diabetes remains a moving target and, hence, a major therapeutic challenge.’
References
1. Luitse MJA, Biessels GJ, Rutten GEHM, et al. Diabetes, hyperglycaemia, and acute ischaemic stroke. Lancet Neurol 2012;11:261–271.
2. Towfighi A, Markovic D, Ovbiagele B. Current national patterns of comorbid diabetes among acute ischemic stroke patients. Cerebrovasc Dis 2012;33:411–418.
3. Fonarow GC, Reeves MJ, Smith EE, et al. Characteristics, performance measures, and in-hospital outcomes of the first one million stroke and transient ischemic attack admissions in get with the guidelines-stroke. Circ Cardiovasc Qual Outcomes 2010;3:291–302.
4. Xian Y, Fonarow GC, Reeves MJ, et al. Data quality in the American Heart Association Get With The Guidelines-Stroke (GWTG-Stroke): results from a national data validation audit. Am Heart J 2012;163:392–398.e1.
5. Fadini GP and Cosentino F. Diabetes and ischaemic stroke: a deadly association. Eur Heart J 2018; published online ahead of print.