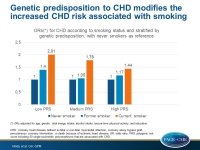
Genetic predisposition modifies the increased CHD risk associated with smoking
The increased CHD risk associated with smoking was higher in those with a lower polygenetic risk score for CHD than with a higher polygenetic risk score.
Polygenic Risk Score for Coronary Heart Disease Modifies the Elevated Risk by Cigarette Smoking for Disease IncidenceLiterature - Hindy G, Wiberg F, Almgren P, et al. - Circ Genom Precis Med. 2018;11:e001856
Introduction and methods
The degree of adverse outcomes in patients with coronary heart disease (CHD) due to cigarette smoking differs between individuals. Smoking modifies the effect of the top single-nucleotide polymorphism (SNP) rs4977574 at the chromosome 9p21 locus, which is the strongest CHD associated locus. Data show that smoking attenuates the increased risk for CHD associated with having 1 or 2 risk alleles [1], but interaction between smoking and a polygenetic risk score (PRS) for CHD has not been tested.
In this study, associations between smoking and incidence of CHD stratified by PRS were investigated, in order to understand, whether smoking interacts with PRS for CHD. Furthermore, it was evaluated whether genetic prediction of CHD differs according to smoking behavior, and interactions between each of the CHD-associated SNPs and smoking on the risk of CHD were tested.
The Malmö Diet and Cancer Study is a population-based prospective study that recruited 30,447 subjects between 1923 and 1950 [2-4]. Baseline data were collected between 1991 and 1996. Subjects with prevalent CHD, those with missing data on smoking, and missing or bad quality DNA were excluded, leaving a study population of 24,443 individuals. Study participants were stratified into 3 smoking categories based on self-reported smoking status: never smokers, former smokers, and current smokers.
A PRS was created from 50 SNPs associated with CHD, indicating levels of genetic predisposition for CHD. Two models were tested: the first including baseline age, sex, education, total energy intake, physical activity, and alcohol consumption (model 1), and the second including model 1 with further adjustments for CHD traditional risk factors (model 2). CHD was defined as fatal or non-fatal myocardial infarction, coronary artery bypass graft, percutaneous coronary intervention, or death because of ischemic heart disease.
Main results
- During a median follow-up period of 19.4 years, 13.2% of participants developed CHD (21.1% of men and 8.3% of women).
- There was a significant association between the PRS and CHD (OR per tertile: 1.31; 95%CI: 1.25-1.37).
- Compared with never smokers, former smokers (OR: 1.19; 95%CI: 1.08–1.31) and current smokers (OR: 1.67; 95%CI: 1.52–1.85) were at increased risk for CHD adjusted for age, gender, total energy intake, alcohol intake, physical activity, and education.
- The increased risk for CHD conferred by smoking was modified by the PRS (Pinteraction=0.005 and 0.009 for model 1 and 2, respectively).
- Compared with never smokers, current smokers in the lowest tertile of PRS had higher CHD risk (OR: 2.01; 95%CI: 1.66–2.42) than current smokers in the highest tertile of PRS (OR: 1.44; 95%CI: 1.23–1.68). A similar but weaker trend was observed among former smokers (ORs for for high/medium/low tertile PRS: 1.4/1.05/1.17, respectively).
- The interaction was stronger among men (Pinteraction=0.001 and 0.001 for model 1 and model 2, respectively) than among women (Pinteraction=0.44 and 0.67 for model 1 and model 2, respectively).
- Adding the PRS to a prediction model that included traditional risk factors improved the discrimination of the model (integrated discrimination improvement, IDI=0.007; P<0.0001). Stratifying by smoking status showed better discrimination by PRS among never smokers (IDI=0.012; P<0.0001) than former smokers (IDI=0.006; P<0.0001) and current smokers (IDI=0.004; P<0.0001).
Conclusion
The increased CHD risk associated with smoking was higher in those with lower PRS than with higher PRS. The PRS for CHD provided better risk discrimination and reclassification on top of traditional risk factors among never smokers compared with smokers.
References
1. Hamrefors V, Hedblad B, Hindy G, et al. Smoking modifies the associated increased risk of future cardiovascular disease by genetic variation on chromosome 9p21. PLoS One. 2014;9:e85893.
2. Callmer E, Riboli E, Saracci R, et al. Dietary assessment methods evaluated in the Malmö food study. J Intern Med. 1993;233:53–57.
3. Wirfält E, Mattisson I, Johansson U, et al. A methodological report from the Malmö Diet and Cancer study: development and evaluation of altered routines in dietary data processing. Nutr J. 2002;1:3.
4. Berglund G, Elmstähl S, Janzon L, et al. The Malmo Diet and Cancer Study. Design and feasibility. J Intern Med. 1993;233:45–51.