More peripheral artery disease patients would benefit from statin therapy
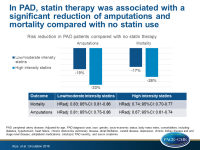
In a large community-based database, in patients with peripheral artery disease, statin therapy was associated with a significant reduction of amputations and mortality compared with no statin use.
Statins Have a Dose-Dependent Effect on Amputation and Survival in Peripheral Artery Disease PatientsLiterature - Arya S, Khakharia A, Binney ZO, et al. - Circulation. 2018;137:1435-1446
Introduction and methods
Peripheral artery disease (PAD) is associated with significant disability, morbidity and mortality, but risk factor modification is poor for this condition, relative to CAD or stroke [1,2]. ACC/AHA 2013 guidelines recommend high-intensity statin therapy for all clinically apparent atherosclerotic cardiovascular disease, but indicate that the level of evidence for PAD is low [3].
This study evaluated the effect of statin intensity on PAD outcomes of amputation and mortality. Moreover, variation in prescription of statin intensity over time and presence of comorbid atherosclerotic disease conditions was assessed in a large PAD cohort. For this purpose, incident PAD patients were identified in the national Veterans Health Administration (VHA) database between 2003 and 2014, and stratified in those without statin therapy (active comparator group), those on low/moderate intensity statin therapy, and those on high intensity statin therapy within 1 year of diagnosis. Statin exposure was defined as the highest statin dose prescribed.
Outcomes of interest were incident amputation and death. The results were adjusted for age, PAD diagnosis year, race, gender, socio-economic status, body mass index, comorbidities, including diabetes, hypertension, heart failure, chronic obstructive pulmonary disease, atrial fibrillation, carotid disease, depression, chronic kidney disease and end stage renal disease, antiplatelet medication, cilostazol, PAD severity, and serum creatinine.
Main results
- 155,647 patients were identified and followed-up for a median of 5.9 years.
- 28% of patients were not on statin treatment. This percentage remained steady throughout the study. 38.8% were on low/moderate intensity statins and 12.4% on high intensity statin therapy.
- 20.9% were on simvastatin 80 mg at the beginning of follow-up. Use of simvastatin 80 mg declined, and the use of high-intensity statins increased over time.
- PAD patients with comorbidities were more likely to receive statin therapy. Those with CAD, carotid disease and PAD had a higher likelihood of receiving high intensity statin, compared with those with PAD only (18.4% vs 6.4%).
- The use of low/moderate intensity statins was associated with a 17% decrease in mortality (HRadj: 0.83; 95%CI: 0.81-0.86), and the use of high intensity statins was associated with a 26% decrease in mortality (HRadj: 0.74; 95%CI: 0.70-0.77).
- The use of low/moderate intensity statins was associated with a 19% lower amputation risk (HR: 0.81; 95%CI: 0.75-0.86), and the use of high intensity statins with a 33% lower amputation risk (HR: 0.67; 95%CI: 0.61-0.74).
Conclusion
Statins are underutilized in PAD patients. In a large community-based database, statin therapy was associated with a significant reduction of amputations and mortality in this patient group, compared with no statin use. The benefit observed was higher with higher intensity statins.
Editorial comment
In their editorial article, Aday and Everett [4] emphasize that the publication of Arya et al is able to address important open questions, including the associations between statin intensity and amputations, as well as death in PAD patients. They discuss the study limitations including additional unidentified confounders, the lack of a time-varying analysis of statin use changes after the 1st year, and the fact that additional interventions, like smoking cessation, were not taken into account. They also suggest that it would be interesting to use two separate active comparator groups, one on aspirin alone and one on clopidogrel alone.
The authors conclude: ‘The report by Arya and colleagues adds to a growing literature documenting the underuse of statin therapy in patients with PAD. They have also demonstrated a strong, intensity-dependent effect on amputation and mortality, 2 outcomes of clear importance for both patients and physicians. “
The importance of these medications in preserving both life and limb deserves more attention of health care providers and payer, to enhance the rates of use and adherence to high intensity statin therapy in this large and growing population of patients with PAD.
References
1. Pereg D, Neuman Y, Elis A, et al. Comparison of lipid control in patients with coronary versus peripheral artery disease following the first vascular intervention. Am J Cardiol. 2012;110:1266-1269.
2. Hira RS, Cowart JB, Akeroyd JM, et al. Risk Factor Optimization and Guideline-Directed Medical Therapy in US Veterans With Peripheral Arterial and Ischemic Cerebrovascular Disease Compared to Veterans With Coronary Heart Disease. Am J Cardiol. 2016;118:1144-1149.
3. Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S1-S45.
4. Aday AW and Everett BM. Statins in Peripheral Artery Disease: What Are We Waiting For? Circulation. 2018;137:1447-1449.