Total cholesterol levels determine survival in homozygous FH
In a retrospective survey of 133 patients with HoFH, the total serum cholesterol achieved by lipid-lowering therapies, was a major determinant of survival.
Survival in homozygous familial hypercholesterolaemia is determined by the on-treatment level of serum cholesterolLiterature - Thompson GR, Blom DJ, Marais AD, et al. - Eur Heart J 2018; published online ahead of print
Introduction and methods
Homozygous FH is associated with premature CV death and major adverse cardiovascular events (MACE), with an average age of death of 18 years, if not treated [1-4]. Lipid-lowering therapy is recommended for these patients, however, there are no randomized clinical trials showing the benefits of this therapy.
In this retrospective survey, lipid levels and clinical outcomes were assessed in South African and UK FH homozygotes treated with various lipid-lowering measures between 1990 and 2014. For this purpose, 133 patients were included, who were alive and statin-naive at the start of 1990, and were retrospectively followed up until death or the end of 2014. The outcomes that were compared between groups were death from any cause, CVD death, and fatal plus nonfatal MACE.
Most patients were treated initially with maximal doses of simvastatin, or atorvastatin (after 1997), or rosuvastatin (after 2003), and more than 50% of patients received additionally ezetimibe from 2004 onwards. Other treatments were apheresis (from 1990), lomitapide (from 2008), and evolocumab (from 2012).
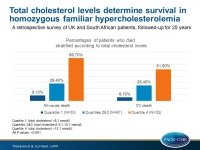
Patients were divided into 3 groups based on quartiles of on treatment total cholesterol (TC):
- Quartile 1: TC <8.1 mmol/L (N=33)
- Quartiles 2+3: TC 8.1-15.1 mmol/L (N=67)
- Quartile 4: TC >15.1 mmol/L (N=33)
Main results
- The percentages of patients receiving lipid-lowering therapies in quartile 1 were higher compared with quartile 4: for apheresis 24% vs. 18%; P=0.70, for statins 100% vs. 88%; P=0.03, for ezetimibe 55% vs. 33%; P=0.006, and for evolocumab 33% vs. 9%; P=0.05.
- The percentages of patients who died were lower in patients with lower TC levels. The percentages of any death were 9.1% in quartile 1, 28.4% in quartiles 2 and 3, and 69.7% in quartile 4, whereas the corresponding percentages for CV death were 6.1%, 25.4% and 51.5% (all P values <0.001).
- After adjusting for pre-treatment TC levels, demographic characteristics, and differences in therapy, patients in quartile 4 had still a 6-fold increased risk of death compared with those in quartile 1 (P=0.04).
- The risk of MACE was approximately twice as high in quartile 4 compared with quartile 1 (P=0.01), but the hazard ratios became statistically insignificant after adjustment for confounding factors.
Conclusion
In a retrospective survey of 133 FH patients, the TC achieved by lipid-lowering therapies, was a major determinant of survival. These findings suggest that aggressive lipid-lowering therapies must be implemented for these patients.
Editorial comment
In their editorial article [5], Stoekenbroek, Hovingh, and Kastelein, comment that the findings of the study of Thompson et al are very convincing, despite the limitations of the study, including the limited sample size, the differences in patient characteristics, and the retrospective nature of the survey. They discuss several promising treatment options, including evinacumab, a monoclonal antibody targeting ANGPTL3 and not dependent on LDL receptor activity, gemcabene, which reduces the synthesis of hepatic cholesterol, triglycerides and apoC3, and finally gene therapy with a virus vector carrying the LDL receptor gene. The authors conclude: ‘HoFH remains a devastating disease and its consequences can only be limited by early initiation of multimodal treatment. The combination of high-dose statins, ezetimibe, and evolocumab has substantially improved outcomes for these patients, although even this combination enables only a minority of patients to reach acceptable lipid levels. Thompson et al. have now confirmed that the extent of therapeutic cholesterol reduction determines survival in HoFH patients. This conclusion underlined the need for a rigorous, multimodal treatment approach, often including apheresis, until the promising therapies which are under development become available.’
References
1. Rallidis L, Naoumova RP, Thompson GR, et al. Extent and severity of atherosclerotic involvement of the aortic valve and root in familial hypercholesterolaemia. Heart 1998;80:583–590.
2. Alonso R, Dıaz-Dıaz JL, Arrieta F, et al. Clinical and molecular characteristics of homozygous familial hypercholesterolemia patients: Insights from SAFEHEART registry. J Clin Lipidol 2016;10:953–961.
3. Thompson GR, Miller JP, Breslow JL. Improved survival of patients with homozygous familial hypercholesterolaemia treated with plasma exchange. Br Med J Clin Res Ed 1985;291:1671–1673.
4. Raal FJ, Pilcher GJ, Panz VR, et al. Reduction in mortality in subjects with homozygous familial hypercholesterolemia associated with advances in lipid lowering therapy. Circulation 2011;124:2202–2207.
5. Stoekenbroek RM, Hovingh GK, and Kastelein JJP. Homozygous familial hypercholesterolaemia: light at the end of the tunnel. Eur Heart J 2018; published online ahead of print.