Pneumococcal and influenza infections associated with higher risk of CV events
Individuals with at least one laboratory-confirmed respiratory infection had a higher risk of MI or stroke, in particular when infected with S. pneumoniae or influenza virus.
Laboratory-confirmed respiratory infections as triggers for acute myocardial infarction and stroke: a self-controlled case series analysis of national linked datasets from ScotlandLiterature - Warren-Gash C, Blackburn R, Whitaker H, et al. - Eur Respir J 2018; 51: 1701794
Introduction and methods
Acute respiratory tract infections are associated with a short-term increase in the risk of acute CV events [1]. Influenza virus and S. pneumoniae have direct myocardial effects and may exacerbate underlying atherosclerotic disease, however the effects of specific organisms is not clear [2]. A meta-analysis of data comparing influenza vaccine versus placebo in people with existing CVD shows a 36% reduction in the risk of major adverse cardiovascular events associated with influenza vaccination [3]. Moreover, the receipt of pneumococcal vaccine was associated with a modest cardio-protective effect [4].
In this study, the association between laboratory-confirmed respiratory bacteria or virus infections and risk of first myocardial infarction (MI) or stroke was quantified, using self-controlled case series analysis of anonymized linked electronic health records from Scotland in the UK.
For this purpose, the following data sources were used:
- the general/acute hospital inpatient data from the Scottish Morbidity Record (SMR01), a large national dataset with more than 1.4 million records per year
- the Electronic Communication of Surveillance in Scotland (ECOSS) dataset, with information on all identifications of organisms or infections of clinical and public health significance
All individuals aged ≥40 years, with a hospital admission for MI or stroke from 2004-2014 were identified in the SMR01. All linked ECOSS records were searched for positive tests for influenza virus, parainfluenza virus, rhinovirus, respiratory syncytial virus, human meta-pneumo-virus or S. pneumoniae during the same study period. Individuals with a record of first MI or stroke and a record of at least one laboratory-confirmed respiratory infection were included in the analysis (N=1989).
Main results
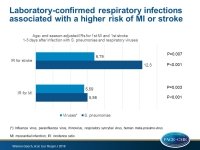
- The adjusted IR for first MI was significantly increased in the first 1–3 days after both respiratory bacterial and viral infections (IR for S. pneumoniae: 5.98; 95%CI: 2.47–14.4; P<0.001; IR for viruses: 5.59; 95%CI: 1.77–17.6; P=0.003), and persisted for approximately 1 week.
- The adjusted IR for first stroke was 12.3 for S. pneumoniae (95%CI: 5.48–27.7; P<0.001) and 6.79 for viruses (95%CI: 1.67–27.5; P=0.007) for days 1–3. Elevated rates of stroke following both bacterial and viral infections persisted to 28 days (P<0.001).
- Influenza virus infections were associated with higher IRs for both MI and stroke compared with all other respiratory viruses combined.
- The MI adjusted day 1–3 IR for influenza virus was 9.80 (95%CI: 2.37–40.5) and for other respiratory viruses it was 2.81 (95%CI: 0.39–20.3).
- The stroke adjusted day 1–3 IR after influenza virus was 7.82 (95%CI: 1.07–56.9) and for other respiratory viruses it was 4.86 (95%CI: 0.67–35.4).
- Individuals aged <65 years tended to have higher adjusted IRs for MI and stroke after respiratory bacteria and virus infections than those aged ≥65 years, although CIs were overlapping.
Conclusion
Individuals with at least one laboratory-confirmed respiratory infection had a higher risk of MI or stroke, in particular when infected with S. pneumoniae or influenza virus. These results suggest that pneumococcal and influenza vaccines may be useful in the prevention of CV events.
References
1. Corrales-Medina VF, Suh KN, Rose G, et al. Cardiac complications in patients with community-acquired pneumonia: a systematic review and meta-analysis of observational studies. PLoS Med 2011; 8: e1001048.
2. Singanayagam A, Singanayagam A, Elder DHJ, et al. Is community-acquired pneumonia an independent risk factor for cardiovascular disease? Eur Respir J 2012; 39: 187–196.
3. Udell JA, Zawi R, Bhatt DL, et al. Association between influenza vaccination and cardiovascular outcomes in high-risk patients: a meta-analysis. JAMA 2013; 310: 1711.
4. Ren S, Newby D, Li SC, et al. Effect of the adult pneumococcal polysaccharide vaccine on cardiovascular disease: a systematic review and meta-analysis. Open Heart 2015; 2: e000247.