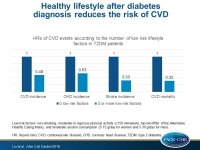
Healthy lifestyle after diabetes diagnosis reduces risk of CVD
Maintaining or changing to a healthy lifestyle after diabetes diagnosis is associated with a significantly lower risk CVD incidence and mortality.
Influence of Lifestyle on Incident Cardiovascular Disease and Mortality in Patients With Diabetes MellitusLiterature - Liu G, Li Y, Hu Y, et al. - J Am Coll Cardiol 2018;71:2867–76
Introduction and Methods
Lifestyle interventions, including high quality nutrition, smoking cessation, and physical activity, reduce the risk of CVD in general populations, as well as the risk of type 2 diabetes (T2DM), but it is not clear to what degree they limit the CVD risk after a T2DM diagnosis
[1].
In this analysis of 2 large prospective cohort studies of T2DM patients, healthy lifestyle practices after diabetes diagnosis and lifestyle factors before and after diabetes diagnosis were prospectively evaluated, and their associations with the subsequent risk of CVD incidence and CVD mortality were assessed.
For this purpose, participants in the Nurses’ Health Study (NHS) and the Health Professionals Follow-Up Study (HPFS) with incident diabetes diagnosed during follow-up were enrolled (1980-2012) [2]. Findings were self-reported based on questionnaires that were assessed every 2-4 years. Those with T2DM, CVD, or cancer at baseline, as well as those with CVD before T2DM diagnosis or missing data were excluded, leaving a sample of 8,970 women in the NHS and 2,557 men in the HPFS with an average follow-up of 13.3 years.
The 4 modifiable lifestyle factors studied were diet, smoking status, alcohol consumption and physical activity. The quality of diet was evaluated based on the 2010 Alternate Healthy Eating Index (AHEI) score, and a low risk diet was defined by the top two-fifths of AHEI [3]. Physical activity was defined as low risk when there was ≥150 min/week of ≥3 metabolic equivalents activity, and alcohol consumption was defined as low risk with 5-15 g/day for women and 5-30 g/day for men. For each low-risk lifestyle factor, one point was given if the study participant met the criterion for the low-risk category, or zero points otherwise.
The outcomes were CVD mortality and CVD incidence, defined as fatal and non-fatal stroke, and fatal and non-fatal coronary heart disease (CHD), including coronary artery bypass graft surgery and non-fatal myocardial infarction (MI).
Main results
- Compared with a 0 low-risk lifestyle factor, participants with ≥3 low-risk lifestyle factors had HRs of 0.48 (95%CI: 0.40-0.59) for total CVD incidence, 0.53 (95%CI: 0.42-0.66) for CHD incidence, 0.33 (95%CI: 0.21-0.51) for stroke incidence, and 0.32 (95%CI: 0.22-0.47) for CVD mortality (all P trend <0.001).
- The population-attributable risk for poor adherence to an overall healthy lifestyle (<3 low-risk factors) was 40.9% (95%CI: 28.5%-52.0%) for CVD mortality.
- Compared to no changes in lifestyle, participants who improved their lifestyle after the diabetes diagnosis had an HR of 0.79 (95%CI: 0.70-0.89) for total CVD incidence, 0.82 (95%CI: 0.72-0.94) for CHD incidence, 0.68 (95%CI: 0.52-0.89) for stroke incidence, and 0.80 (95%CI: 0.66-0.96) for CVD mortality (all P trend <0.001).
- For each number increment in low-risk lifestyle factors, there was a 14% lower risk of total CVD incidence, a 12% lower risk of CHD incidence, a 21% lower risk of stroke incidence, and a 27% lower risk of CVD mortality (all P< 0.001).
- Compared with maintaining a lifestyle score<2 after the diabetes diagnosis, participants who changed the lifestyle score from <2 to ≥2 after diabetes diagnosis had a 19% (95%CI: 8%-29%) lower risk of CVD incidence and a 20% (95%CI: 2%-34%) lower risk of CVD mortality.
Conclusion
Maintaining or changing to a healthy lifestyle after diabetes diagnosis is associated with a significantly lower risk of CVD incidence and CVD mortality. The greater the number of lifestyle improvements, the lower the CVD risk. These findings support the healthy lifestyle recommendations for T2DM patients.
Editorial comment
In their editorial article, Connelly, Ghandi, and Horton [4] summarize the findings of Liu et al, and discuss the study limitations that include the homogeneity of the study population, consisting of health care professionals of high socioeconomic status, mainly Caucasian, the fact that participation in the study was voluntary, suggesting that participants were more adherent to implement lifestyle changes, and the use of questionnaires and self-reported findings, whose validity and reproducibility might be questionable. The authors conclude: ‘Lifestyle intervention in patients with T2DM remains low risk, cost effective, and relatively easy to integrate into health care delivery models. Despite this, important questions remain unanswered: which diet(s) are best? What quantity of alcohol is safe in this cohort? Is there a “minimum” or “maximum” amount of exercise and is the type of exercise important? How do we monitor compliance? Who should write the diet and exercise prescription—physicians or other health care professionals? How generalizable are these findings to other groups of different ethnicity and/or socioeconomic status? As practitioners managing patients with T2DM, we need to send a clear message that health care promotion, advocacy, and research should continue to focus on these healthy lifestyle factors not only to improve glycemic control, but to reduce overall cardiovascular risk. As society continues to evolve and becomes increasingly complex, it is important that we do not overlook the so-called simple and fundamental aspects of patient care and always return “back to basics.”
References
1. Loef M, Walach H. The combined effects of healthy lifestyle behaviors on all cause mortality: a systematic review and meta-analysis. Prev Med 2012;55:163–70.
2. Colditz GA, Manson JE, Hankinson SE. The Nurses’ Health Study: 20-year contribution to the understanding of health among women. J Womens Health 1997;6:49–62.
3. Chiuve SE, Fung TT, Rimm EB, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr 2012;142:1009–18.
4. Connelly K, Gandhi S, Horton E. Lifestyle and CV Risk in Patients With Diabetes. Time to Get “Back to Basics”. J Am Coll Cardiol 2018;71:2877-79.