Reduced CV risk with intensive blood pressure treatment in T2DM patients on standard glycemic control
In a subanalysis of the ACCORD BP trial, intensive blood pressure treatment in T2DM patients receiving standard glycemic control was significantly associated with a decreased risk of CV events, including HF hospitalization.
Benefits of Intensive Blood Pressure Treatment in Patients With Type 2 Diabetes Mellitus Receiving Standard but Not Intensive Glycemic ControlLiterature - Tsujimoto T and Kajio H. - Hypertension. 2018;72: published online ahead of print
Introduction and methods
The Action to Control Cardiovascular Risk in Diabetes Blood Pressure (ACCORD BP) study showed that treating high risk type 2 diabetes (T2DM) patients to the intensive systolic blood pressure (BP) target of<120 mm Hg, did not lead to a reduction in fatal and non-fatal major CV events, compared with patients treated to the systolic BP target of <140 mm Hg [1-3]. However, CV events did not include heart failure (HF), and hypoglycemic events were not taken into account.
This subanalysis of the ACCORD BP trial evaluated whether intensive BP treatment, compared with standard BP treatment, is beneficial in preventing CV events, including HF, in patients receiving either standard or intensive glycemic control.
In the ACCORD study, 10,251 T2DM patients aged 40-79 years with established CVD, or aged 55-79 years with a high CV risk, were randomly assigned to standard glycemic control (target glycohemoglobin 7.0%–7.9%) or to intensive glycemic control (target glycohemoglobin<6.0%). On top of that, ACCORD BP participants were randomly assigned to standard BP treatment (target systolic BP <140 mm Hg) or to intensive BP treatment (target systolic BP <120 mm Hg).
The primary outcome for the present analysis was the composite of CV death, non-fatal myocardial infarction, non-fatal stroke, and hospitalization for congestive HF. The secondary outcomes included all-cause death, major coronary events (fatal coronary heart disease, non-fatal myocardial infarction, or unstable angina), stroke (fatal or non-fatal), and HF (fatal or hospitalized congestive HF).
Main results
- In the present analysis 4,733 eligible patients were followed-up for a mean of 4.5±1.4 years.
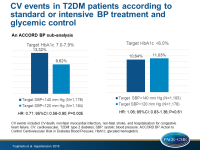
- In the standard glycemic control group, the risk of the primary endpoint was significantly lower in the intensive BP treatment group compared to the standard BP treatment group (9.62% vs 13.32%; 21.1 vs 29.7/1,000 person-years; HR: 0.71; 95%CI: 0.56–0.90; P=0.005).
- In the intensive glycemic control group, the risk of the primary endpoint did not differ significantly between the intensive and the standard BP treatment groups (11.93% vs 10.64%; 24.9 vs 23.2/1,000 person-years; HR: 1.06; 95%CI: 0.83–1.36; P=0.61).
- There was significant interaction between BP treatment strategy and glycemic control for the primary outcome (P for interaction=0.02).
- The risk of stroke in patients receiving standard glycemic control was significantly lower in the intensive BP treatment group compared with the standard BP treatment group (HR: 0.49; 95%CI: 0.27–0.87; P=0.01).
- The risk of stroke in patients receiving intensive glycemic control was not significantly different between the two BP treatment groups and the same was true for other secondary outcomes.
- All-cause mortality in patients receiving intensive glycemic control was nonsignificantly higher in patients receiving intensive BP treatment compared to those receiving standard BP treatment (HR: 1.38; 95% CI, 0.99–1.92; P=0.05).
Conclusion
Intensive BP treatment in T2DM patients receiving standard glycemic control was associated with a significant decreased risk of CV events, including HF hospitalization, which was not the case in patients on intensive glycemic control.
Editorial comment
In their editorial article, Kjeldsen, Os, and Nilsson [4] criticize the analysis of Tsujimoto et al. of being statistically underpowered, meaning that the findings may represent a play of chance. On the other hand, they discuss a plausible explanation for their results: Severe hypoglycemia episodes may have raised the risk for major CV adverse events in the intensive glycemic control group, thus, negating the benefit resulting from intensive BP control.
The authors conclude: ‘The new ACCORD analysis is another strong argument for launching one or more interventional trial with appropriate study design and sufficient statistical power that may convincingly clarify whether a systolic BP target <120 mm Hg prevents cardiovascular complications in patients with diabetes mellitus. Until such data appear from the ACCORD study organization, or from others, the target systolic BP in patients with diabetes mellitus remains 130/80 mm Hg as now stated in both the American and European hypertension guidelines.’
References
1. Buse JB, Bigger JT, Byington RP, et al. Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial: design and methods. Am J Cardiol. 2007;99(12A):21i–33i.
2. Gerstein HC, Riddle MC, Kendall DM, et al; ACCORD Study Group. Glycemia treatment strategies in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Am J Cardiol.2007;99(12A):34i–43i.
3. Gerstein HC, Miller ME, Ismail-Beigi F, et al; ACCORD Study Group. Effects of intensive glycaemic control on ischaemic heart disease: analysis of data from the randomised, controlled ACCORD trial. Lancet. 2014;384:1936–1941.
4. Kjeldsen SE, Os I, Nilsson PM. Does Intensive Glucose Control Cancel Out Benefits of Systolic Blood Pressure Target <120 mm Hg in Patients With Diabetes Mellitus Participating in ACCORD? Hypertension. 2018;72: published online ahead of print.