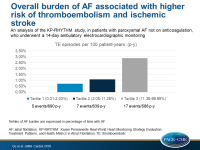
Overall burden of AF associated with higher risk of thromboembolism and ischemic stroke
Longer total time spent in AF was associated with a higher risk of thromboembolism and ischemic stroke in adults with paroxysmal AF, who were not on anticoagulation, independent of known stroke risk factors.
Association of Burden of Atrial Fibrillation With Risk of Ischemic Stroke in Adults With Paroxysmal Atrial Fibrillation. The KP-RHYTHM StudyLiterature - Go AS, Reynolds K, Yang J, et al. - JAMA Cardiol. 2018;3(7):601-608
Introduction and methods
Atrial fibrillation (AF) is associated with an increased risk for ischemic stroke (IS) and thromboembolism (TE), but it is not clear whether the risk differs between patients with paroxysmal and non-paroxysmal AF [1,2]. This analysis of the Kaiser Permanente Real-World Heart Monitoring Strategy Evaluation, Treatment Patterns, and Health Metrics in Atrial Fibrillation (KP-RHYTHM) study [3] assessed whether a greater burden of AF is independently associated with the risk of IS and TE, in patients not on anticoagulation.
The retrospective KP-RHYTHM study included a large cohort of patients with paroxysmal AF, confirmed by continuous ambulatory electrocardiographic monitoring (AEM), lasting 14 days with the ZIO XT device (iRhythmTechnologies Inc). For this analysis, adult participants were selected, who underwent AEM between 2001 and 2016, and had confirmed paroxysmal AF, but were not on anticoagulation therapy. The burden of AF was quantified as the percentage of analyzable wear time spent in AF (minimum episode duration: 30 seconds, primary measure), and the longest continuous episode of AF during monitoring (secondary measure). The primary outcome was hospitalization for IS or TE.
Main results
- There were 1,965 eligible patients, with a mean age of 69 (SD: 11.8) years, and 45% were women. The median ATRIA stroke risk score was 4 (IQR: 2-7), and the median CHA₂DS₂-VASc score was 3 (IQR: 1-4).
- AF burden was non-normally distributed (median 4.4%; IQR: 1.1%-17.2%) and the median duration of the longest continuous AF episode was 171 (IQR: 49-590) minutes.
- The unadjusted TE incidence in patients with paroxysmal AF not on anticoagulation therapy was 1.51 per 100 person-years (95%CI: 1.05-2.18).
- There were 5 TE events over 690 person-years in tertile 1 (0.01%-2.03% of time in AF), 7 TE events over 639 person-years in tertile 2 (2.05%-11.28% of time in AF), and 17 TE events over 586 person-years in tertile 3 (11.36%-99.99% of time in AF).
- The unadjusted TE risk in the third tertile of AF burden was 215% higher (HR: 3.15, 95%CI: 1.51-6.61) compared with the first and second tertiles combined.
- Adjustment for TRIA or CHA₂2DS₂2-VASc score did not change the results significantly, and various subgroup analyses revealed no significant interactions.
- The duration of the longest observed AF episode while not on anticoagulation was not significantly associated with the risk of TE, not in the overall population, nor in those without previous ischemic stroke.
Conclusion
In an analysis of the retrospective KP-RHYTHM study, a greater burden of AF, as measured by longer time spent in AF, was associated with a higher risk of IS and TE in adults with paroxysmal AF, who were not on anticoagulation. This finding was independent of known stroke risk factors. The duration of the longest continuous episode of AF during the monitoring period did, however, not predict thromboembolism.
Editorial comment
In their editorial article, Steinberg and Piccini [4] discuss the strengths and the limitations of the study reported by Go et al. The strengths include the long duration of continuous monitoring, the fact that the results describe TE episodes when patients were not on anticoagulation therapy, and the good statistics. The limitations include the choice of one specific monitoring device, possible selection bias since patients had an indication for monitoring but not for anticoagulation, and the fact that the absolute number of events was low. The authors conclude: ‘In summary, the study by Go et al. makes an important contribution to our understanding of the risk of stroke in patients with paroxysmal AF: the burden or volume of AF does matter. It lays solid groundwork for a much-needed clinical trial among these patients with higher overall AF burden and low CHA₂2DS₂2-VASc risk scores.’
References
1. GoAS, Hylek EM, PhillipsKA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors inAtrial Fibrillation (ATRIA) study. JAMA. 2001;285(18):2370-2375.
2. Ganesan AN, Chew DP, Hartshorne T, et al. The impact of atrial fibrillation type on the risk of thromboembolism, mortality, and bleeding: a systematic review and meta-analysis. Eur Heart J. 2016;37(20):1591-1602.
3. Gordon NP. Characteristics of adult health plan members in the Northern California region membership, as estimated from the 2011 Member Health Survey. https://divisionofresearch .kaiserpermanente.org/projects/memberhealthsurvey/SiteCollectionDocuments /mhs11reg.pdf. Accessed February 15, 2018.
4. Steinberg BA, and Piccini JP. When Low-Risk Atrial Fibrillation Is Not So Low Risk. Beast of Burden. JAMA Cardiol. 2018;3(7):published online ahead of print.