Long-term statin adherence inversely associated with all-cause mortality in ASCVD
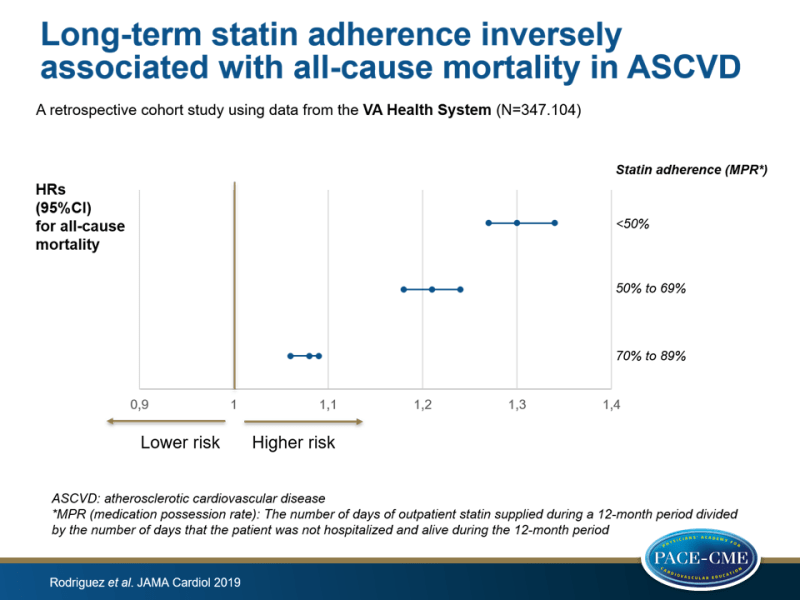
A retrospective cohort study found that low adherence to long-term statin therapy was associated with a higher risk of all-cause mortality in patients with ASCVD.
Association of Statin Adherence With Mortality in Patients With Atherosclerotic Cardiovascular DiseaseLiterature - Rodriguez F, Maron DJ, Knowles JW et al. - JAMA Cardiol 2019; doi:10.1001/jamacardio.2018.4936
Introduction and methods
The updated 2018 American College of Cardiology (ACC)/American Heart Association (AHA) cholesterol guidelines recommend statins as main therapy for patients with atherosclerotic cardiovascular disease (ASCVD) and emphasize the importance of determining adherence in routine follow-up [1]. However, statins are substantially underused and underdosed in many high-risk patients, even after an acute coronary syndrome [2-4]. The reasons for low adherence to statin treatment are complex and may include patient, clinician, and health care system factors that remain unclear. Further, most studies evaluated statin adherence in patients immediately after an ASCVD event or hospitalization during which new statins were prescribed.
This retrospective cohort study (n=347.104) therefore determined the association between statin adherence and all-cause mortality for outpatients with established ASCVD (aged 18-85 years) within the Veterans Affairs (VA) Health System (January 2013 – April 2014) who had a stable statin prescription, and investigated whether this association was modified by statin intensity or by patient-level or by system-level characteristics. Patients who underwent dose reduction or intensification during the 6 months after the index date were excluded. Statin intensity was categorized according to the ACC/AHA cholesterol treatment guidelines: low, moderate or high [1,5]. Adherence was defined by the medication possession ratio (MPR), which was calculated by dividing the number of days of outpatient statin supplied during a 12-month period by the number of days that the patient was not hospitalized and alive during the 12-month period. MPR was classified as: <50%, 50% to 69%, 70% to 89%, or ≥90%. Mean follow-up was 2.9 years.
Primary outcome was all-cause mortality. Secondary outcomes were 1-year mortality, 1-year hospitalization for ischemic heart disease or ischemic stroke.
Main results
Patient characteristics and adherence to statin therapy
- Mean statin adherence to stable statin therapy was 87.7%.
- Those taking moderate-intensity statin treatment were slightly more likely to adhere, compared with those taking low-intensity or high-intensity statin therapy (OR: 1.18, 95%CI: 1.16-1.20, P<0.001).
- Women were less likely to adhere to statin therapy vs men (OR: 0.89, 95%CI: 0.84-0.94, P<0.001), as were minority race groups vs. non-Hispanic white patients.
- Younger and older patients were less adherent, compared with those aged 65-74 years.
Adherence to statin therapy and 1-year hospitalization
- After multivariable adjustment, the OR for 1-year hospitalization for ischemic heart disease or ischemic stroke was 1.08 (95%CI: 1.03-1.14) for those with MPR <50%, 1.02 (95%CI: 0.99-1.07) for MPR 50%-69%, and1.09 (95%CI: 1.06-1.12) for MPR 70%-89% (all P<0.001), compared to those with an MPR ≥90%.
Adherence to statin therapy and 1-year all-cause mortality
- After multivariable adjustment, adherence levels were significantly associated with 1-year mortality. Patients with an MPR <50% had an HR for 1-year mortality of 1.30 (95%CI: 1.27-1.34), compared with the most adherent patients (MPR ≥90%). Those with an MPR of 50%-69% had an HR of 1.21 (95%CI: 1.18-1.24), and those with an MPR 70%-89% had an HR of 1.08 (95%CI: 1.06-1.09). The effect size was attenuated but remained significant after adjustment for LDL-c levels.
- A graded association between drug adherence and mortality was found. This gradation was greatest for those on high-intensity statin therapy.
Conclusion
This retrospective cohort study showed an inverse, graded association between long-term statin adherence and all-cause mortality in VA patients with ASCVD. These data suggest that optimization of statin adherence is needed to improve secondary prevention of ASCVD.
References
1. Grundy SM, Stone NJ, Bailey AL, et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/ APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published online November 2018]. J Am Coll Cardiol. 2018. doi:10.1016/j.jacc.2018.11.003
2. Hirsh BJ, Smilowitz NR, Rosenson RS, Fuster V, Sperling LS. Utilization of and adherence to guideline-recommended lipid-lowering therapy after acute coronary syndrome: opportunities for improvement. J AmColl Cardiol. 2015;66(2):184-192. doi:10.1016/j.jacc.2015.05.030
3. Maddox TM, Borden WB, Tang F, et al. Implications of the 2013 ACC/AHA cholesterol guidelines for adults in contemporary cardiovascular practice: insights from the NCDR PINNACLE registry. J AmColl Cardiol. 2014;64(21): 2183-2192. doi:10.1016/j.jacc.2014.08.041
4. Rosenson RS, Kent ST, Brown TM, et al. Underutilization of high-intensity statin therapy after hospitalization for coronary heart disease. J AmColl Cardiol. 2015;65(3):270-277. doi:10.1016/j.jacc.2014.09.088
5. Stone NJ, Robinson JG, Lichtenstein AH, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J AmColl Cardiol. 2014;63(25 Pt B):2889-2934. doi:10.1016/j.jacc.2013.11.002
