Causal association of LCL-c with ischemic stroke and intracerebral hemorrhage
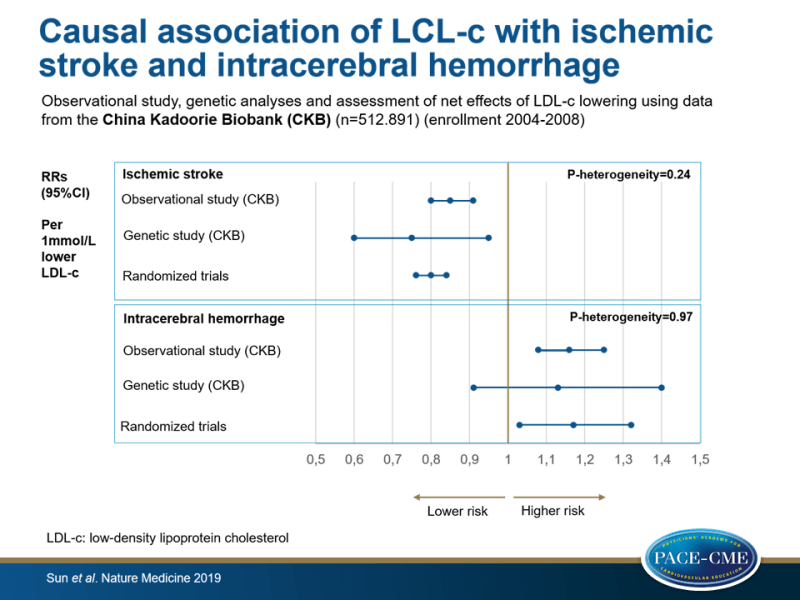
Observational and genetic analyses found a causal positive association of LDL-c with ischemic stroke and a causal negative association with ICH in a Chinese population. Using randomized trial data, a net benefit for the prevention of overall stroke with lowering LDL-c was shown.
Causal associations of blood lipids with risk of ischemic stroke and intracerebral hemorrhage in Chinese adultsLiterature - Sun L, Clarke R, Bennett D et al. - Nature Medicine 2019; https://doi.org/10.1038/s41591-019-0366-x
Introduction and methods
Despite lower LDL-c concentrations in Chinese populations, stroke incidence and intracerebral hemorrhage (ICH) proportions are higher in China, compared to Western populations. The link between LDL-c levels and both stroke types remains unclear. Observational data have demonstrated weaker positive associations of LDL-c with ischemic stroke (IS), compared to coronary heart disease (CHD) [1,2], while LDL-c lowering trials have shown similar risk reduction for IS and CHD [3-5]. Mendelian randomization studies of LDL-c and IS have reported contradictory data [6-8]. Concerns about the excess risks of ICH linked to lowering LDL-C [9,10] may have prevented the more widespread use of statins in China.
The China Kadoorie Biobank (CKB) study recruited 512.891 adults aged 30–79 years from 10 diverse areas in China during 2004–2008. First, the associations between biochemically measured lipids and brain image-confirmed stroke were assessed in a nested case-control study in the CKB, which included 5.475 individuals with IS, 4.776 with ICH, and 6.290 healthy controls (enrollment 2004-2008). For this nested case-control study, adults were selected who had no prior history of stroke, CHD, or cancer, and did not receive lipid-lowering, anticoagulant, or antiplatelet therapy at baseline.
Second, genetic analyses in the same nested population were done to study whether the association of LDL-c with risk of IS and ICH was causal. Based on results of Mendelian randomization trials, a genetic risk score (GRS) comprising 46 single-nucleotide polymorphisms most significantly associated with plasma LDL-c levels in the Global Lipids Genetics Consortium [11,12] was calculated for each CKB participant.
Third, net effects of LDL-c lowering were assessed in all CKB participants by applying relative risk estimates from a meta-analysis of LDL-c lowering trials to the age-specific absolute risks of stroke types and major coronary events (MCEs, including MI and fatal ischemic heart disease). LDL-c lowering trials were identified if they assessed an unconfounded intervention to reduce LDL-c levels, had scheduled duration ≥2 years, and included ≥1.000 participants, leaving 7 trials. Net effects were calculated for total population and per risk level. Low-risk (n=336.696) was defined as no hypertension or prior history of CVD, medium risk (n=153.066) as hypertension without prior history of CVD, and high risk (n=23.129) as hypertension and prior history of CVD.
Main results
Observational data on the association of lipids with risk of stroke types
- After multivariable analysis, each 1 mmol/L higher LDL-c was positively linked to a risk of IS (RR: 1.17, 95%CI: 1.10-1.25) and inversely linked to a risk of ICH (RR: 0.86, 95%CI: 0.80-0.92). This translated into an RR of 0.85 (95%CI: 0.80-0.91) for IS and an RR of 1.16 (95%CI: 1.08-1.25) for ICH, for each 1 mmol/L reduction in LDL-c.
- There was an inverse association of plasma HDL-c levels with risk of IS (RR: 0.93, 95%CI: 0.89-0.97 per 0.3 mmol/L higher HDL-c), but not with ICH (RR: 1.00, 95%CI: 0.96-1.05 per 0.3 mmol/L higher HDL-c).
- Plasma levels of triglycerides were weakly positively associated with a risk of IS (RR: 1.02, 95%CI: 1.00-1.04 per 30% higher triglycerides levels) but were inversely associated with ICH (RR: 0.94, 95%CI: 0.92-0.96).
Genetic data on the association of LDL-c with risk of stroke types
- In the CKB population, the GRS for LDL-c was a strong predictor for plasma LDL-c levels (P=7x10^-247), but not for HDL-c and triglycerides.
- Each 1 mmol/L lower genetically instrumented LDL-c was causally associated with reduced risk of IS (RR: 0.75, 95%CI: 0.60-0.95) and non-significantly higher risk of ICH (RR: 1.13, 95%CI: 0.91-1.40).
Net benefit of LDL-c lowering on overall stroke
- In a meta-analysis of randomized trials of LDL-c lowering drug therapy in worldwide populations, the risk estimates for IS and ICH were RR: 0.80, 95%CI: 0.76-0.84 and RR: 1.17, 95%CI: 1.03-1.32, respectively, per 1 mmol/L lower LDL-c. These estimates were highly consistent with those in the observational and genetic studies of the CKB population (P-heterogeneity=0.24 for IS and P-heterogeneity=0.97 for ICH).
- The predicted number of incident events of IS and MCEs avoided by lowering LDL-c by 1 mmol/L exceeded the predicted number of ICH events per 10.000 Chinese patients treated with statins for 5 years. This observation was independent of age and risk level, showing that both people with and without prior history of CVD benefit from LDL-c lowering in the prevention of overall stroke.
Conclusion
LDL-c was positively associated with IS and equally strong inversely associated with ICH in a study including a large number of brain image-confirmed IS and ICH cases in Chinese populations without prior history of chronic disease or statin use, which was confirmed by genetic analyses in the same population and by a meta-analysis of LDL-c-lowering trials consisting of mostly Western populations. The findings suggest net benefit for the prevention of overall stroke with lowering LDL-c in a Chinese population with high stroke rate, for both primary and secondary prevention settings.
References
1. Lewington, S. et al. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet 370, 1829–1839 (2007).
2. Di Angelantonio, E. et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA 302, 1993–2000 (2009).
3. Collins, R. et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet 388, 2532–2561 (2016).
4. Sabatine, M. S. et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N. Engl. J. Med. 376, 1713–1722 (2017).
5. Ridker, P. M. LDL cholesterol: controversies and future therapeutic directions. Lancet 384, 607–617 (2014).
6. Hopewell, J., Stari, T., Parish, S., Collins, R. & Clarke, R. The impact of genetic variants related to LDL-cholesterol on risk of ischemic stroke and coronary heart disease. Circulation 126, abstr. 11959 (2012).
7. Ference, B. A. et al. Variation in PCSK9 and HMGCR and risk of cardiovascular disease and diabetes. N. Engl. J. Med. 375, 2144–2153 (2016).
8. Hopewell, J. C. et al. Differential effects of PCSK9 variants on risk of coronary disease and ischaemic stroke. Eur. Heart J. 39, 354–359 (2018).
9. Amarenco, P. et al. High-dose atorvastatin after stroke or transient ischemic attack. N. Engl. J. Med. 355, 549–559 (2006).
10. Fulcher, J. et al. Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174,000 participants in 27 randomised trials. Lancet 385, 1397–1405 (2015).
11. Do, R. et al. Common variants associated with plasma triglycerides and risk for coronary artery disease. Nat. Genet. 45, 1345–1352 (2013).
12. Willer, C. J. et al. Discovery and refinement of loci associated with lipid levels. Nat. Genet. 45, 1274–1283 (2013).
