Higher risk of all-cause and cause-specific mortality with low-carbohydrate diets
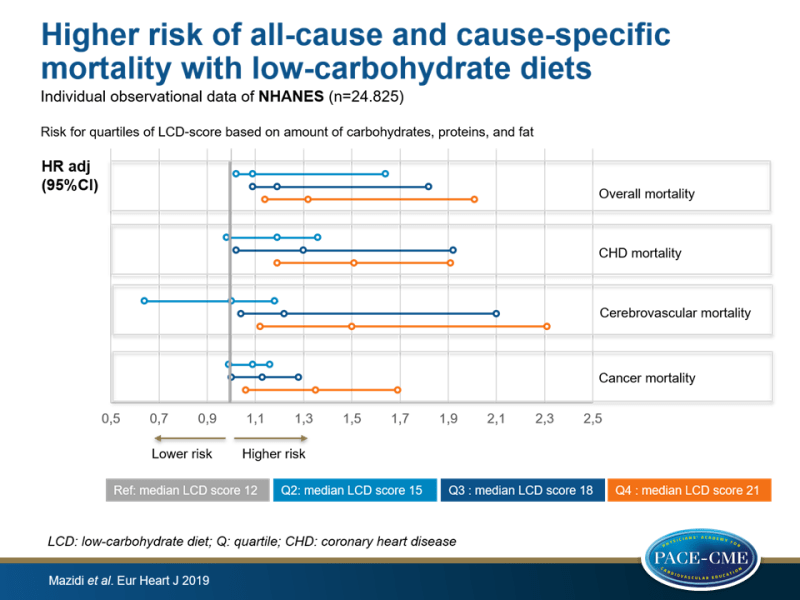
Consumption of low-carbohydrate diets was associated with higher risk of all-cause, CHD, cerebrovascular and cancer mortality in adults, as shown in analyses based on individual and on pooled data.
Lower carbohydrate diets and all-cause and cause-specific mortality: a population-based cohort study and pooling of prospective studiesLiterature - Mazidi M, Katsiki N, Mikhailidis DP et al. - Eur Heart J 2019: doi:10.1093/eurheartj/ehz174
Introduction and methods
Although consumption of low-carbohydrate diets (LCDs) high in protein and fat has been shown to be effective in promoting weight loss and reducing cardiometabolic risk [1,2], long-term safety of LCDs has not yet been clearly reported [3]. Moreover, some studies have suggested increased risk of CVD, overall and cancer morbidity and mortality with LCDs [4-9]. These associations may differ among different study populations [3,4].
Since the evidence is incomplete, and randomized trials to study the effect of LCD on mortality are not feasible, this study aimed to prospectively investigate the link between LCD and all-cause and cause-specific mortality in a large and nationally representative US cohort, as well as by performing a systematic review and meta-analysis of prospective cohort studies on LCD and mortality.
Individual data
Individual data on LCDs and risk of mortality were obtained from the US National Health and Nutrition Examination Survey (NHANES). The current analysis used data from 2-year NHANES survey cycles between 1999-2010, including 24.825 patients aged ≥20 years who were followed for 144 months. Information on dietary consumption was obtained by a trained interviewer, with the use of a computer-assisted dietary interview system and linked to mortality data from Medicare. Endpoints were all-cause mortality, as well as mortality due to coronary heart diseases (CHD), cancer, and cerebrovascular disease. An LCD score was calculated to estimate energy-adjusted intakes of protein, fat, and carbohydrates for each participant, with a maximum score of 30. Consumption of carbohydrates was scored from 10 (lowest consumption) to 0 (highest consumption), whereas protein and fat intake were scored from 0 (lowest consumption) to 10 (highest consumption). Participants were stratified into quartiles, based on LCD score:
- Q1: median LCD score of 12, 367 g carbohydrates/day, 77 g protein/day, 73 g fat/day [reference]
- Q2: median LCD score of 15, 245 g carbohydrates/day, 69 g protein/day, 65 g fat/day
- Q3: median LCD score of 18, 205 g carbohydrates/day, 72 g protein/day, 70 g fat/day
- Q4: median LCD score of 21, 214 g carbohydrates/day, 103 g protein/day, 105 g fat/day
Pooled prospective studies
A meta-analysis of 9 prospective cohort studies (n= 462.934) investigated LCD and risk of overall and cause-specific mortality subsequent to LCD. Inclusion was based on carbohydrate intake being measured with the LCD score, population-based cohort studies and reported overall and cause-specific mortality data, and availability of RR, HR, or OR estimates with 95%CI adjusted for multivariable factors. Participants were >18 years at baseline and did not have prior CHD, diabetes, or any other chronic disease. Mean follow-up was 16.1 years (range: 4.9-29 years).
Main results
Individual data on LCD and mortality (multivariable Cox regression results are presented)
- Results show increased risk of all-cause and cause-specific mortality with higher LCD scores. Note that the amount of carbohydrate consumption did not decrease stepwise with higher LCD scores (i.e. Q3: 205 g/day and Q4: 214 g/day).
- Subjects in Q4 had the highest risk of overall mortality (Q4 HR: 1.32, 95%CI: 1.14-2.01, Q3 HR: 1.19, 95%CI: 1.09-1.82, Q2 HR: 1.09, 95%CI: 1.02-1.64, P-trend<0.001), compared to the Q1 reference.
- Those in Q4 showed an HR of 1.51 (95%CI: 1.19-1.91) for CHD mortality, an HR of 1.50 (95%CI: 1.12-2.31) for cerebrovascular mortality and an HR of 1.35 (95%CI: 1.06-1.69) for cancer mortality, compared to Q1 (all P-trend<0.001).
- Low carbohydrate and high protein consumption was assessed with the LC/HP score. Consuming a LC/HP diet was positively associated with all-cause mortality (HR Q4: 1.21, 95%CI: 1.04-1.39), as well as with CHD (HR Q4: 1.44, 95%CI: 1.02-2.09), cerebrovascular (HR Q4: 1.41, 95%CI: 1.09-1.72), and cancer (HR Q4: 1.22, 95%CI: 1.02-1.48) mortality, compared to reference (all P-trend <0.001).
Pooled prospective data on LCD and mortality
- LCD score was positively associated with all-cause mortality (RR: 1.22, 95%CI: 1.07-1.39, P<0.001 [8 studies, I²=8.6, P=0.912]), CVD mortality (RR: 1.13, 95%CI: 1.02-1.24, P=0.014 [6 studies, I²=11.2, P=0.849]) and cancer mortality (RR: 1.08, 95%CI: 1.01-1.15, P=0.02 [3 studies, I²=10.3, P=0.902]).
- LC/HP diet was positively associated with all-cause mortality (RR: 1.16, 95%CI: 1.07-1.26, P<0.001, no heterogeneity), as well as with CVD (RR: 1.35, 95%CI: 1.07-1.69, P<0.001 [I²=21.5, P=0.736]). In contrast, the relation between LC/HP diet and cancer mortality showed only a trend (RR: 1.03, 95%CI: 0.99-1.07, P=0.084 [I²= 57.3, P=0.036]).
Conclusion
Both individual and pooled data showed an association of LCDs with higher risk of all-cause and cause-specific (CHD, cerebrovascular and cancer) mortality in adults. This raises the question whether these diets should be routinely recommended in clinical practice in light of their short-term weight loss effects, until these potential harmful long-term outcomes have been further evaluated.
According to the authors, potential mechanisms mediating the harmful effects of LCDs may be reduced intake of fiber and fruits, and higher consumption of protein from animal source, cholesterol and saturated fat, which are all risk factors for mortality and CVD [10].
References
1. Clifton PM, Condo D, Keogh JB. Long term weight maintenance after advice to consume low carbohydrate, higher protein diets–a systematic review and metaanalysis. Nutr Metab Cardiovasc Dis 2014;24:224–235.
2. Santos FL, Esteves SS, da Costa Pereira A, et al. Systematic review and meta-analysis of clinical trials of the effects of low carbohydrate diets on cardiovascular risk factors. Obes Rev 2012;13:1048–1066.
3. Nakamura Y, Okuda N, Okamura T, et al. Low-carbohydrate diets and cardiovascular and total mortality in Japanese: a 29-year follow-up of NIPPON DATA80. Br J Nutr 2014;112:916–924.
4. Li S, Flint A, Pai JK, et al. Low carbohydrate diet from plant or animal sources and mortality among myocardial infarction survivors. J Am Heart Assoc 2014;3:e001169.
5. Lagiou P, Sandin S, Weiderpass E, et al. Low carbohydrate-high protein diet and mortality in a cohort of Swedish women. J Intern Med 2007;261:366–374.
6. Trichopoulou A, Psaltopoulou T, Orfanos P, et al. Lowcarbohydrate- high-protein diet and long-term survival in a general population cohort. Eur J Clin Nutr 2007;61:575–581.
7. Fung TT, van Dam RM, Hankinson SE, et al. Lowcarbohydrate diets and all-cause and cause-specific mortality: two cohort studies. Ann Intern Med 2010;153:289–298.
8. Sjogren P, Becker W, Warensjo E, et al. Mediterranean and carbohydrate-restricted diets and mortality among elderly men: a cohort study in Sweden. Am J Clin Nutr 2010;92:967–974.
9. Nilsson LM, Winkvist A, Eliasson M, et al. Low-carbohydrate, high-protein score and mortality in a northern Swedish population-based cohort. Eur J Clin Nutr 2012;66:694–700.
10. McCullough ML, Feskanich D, Stampfer MJ, et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr 2002;76:1261–1271.
