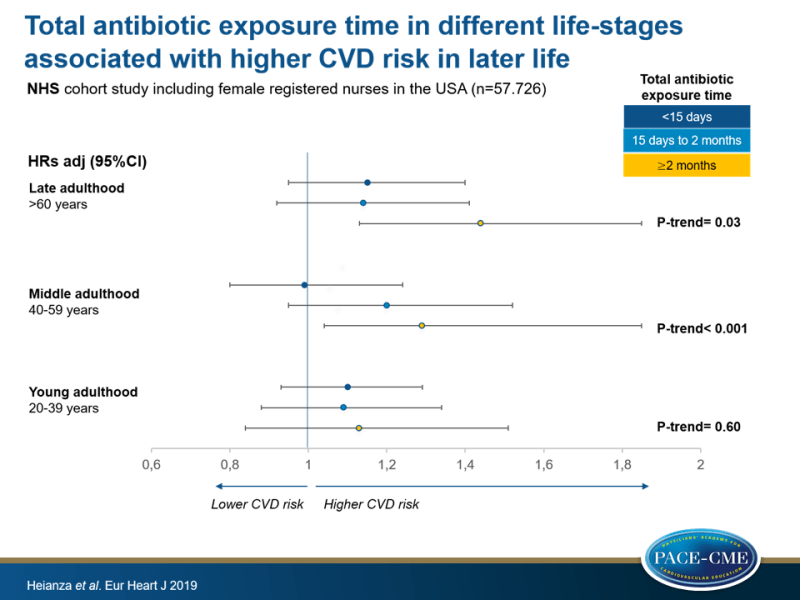
Total antibiotic exposure time in different life-stages associated with higher CVD risk in later life
In women, longer total exposure to antibiotics in middle- and late adulthood was significantly associated with risk of CVD in later life, and antibiotic use in middle adulthood with risk of CHD but not of stroke.
Duration and life-stage of antibiotic use and risk of cardiovascular events in womenLiterature - Heianza Y, Zheng Y, Ma W et al. - Eur Heart J 2019; doi:10.1093/eurheartj/ehz231
Introduction and methods
Antibiotic exposure is suggested to be associated with imbalanced and changed composition of gut microbiota [1-3], which is linked to cardiometabolic abnormalities [4]. Use of macrolide antibiotics has been shown to be positively linked with CV and sudden cardiac death [5-16].
A meta-analysis found higher risk of sudden cardiac death, ventricular tachyarrhythmias, and CV mortality with macrolide antibiotic use (for 3 days to 1 year) [5]. Another study showed increased risk of myocardial infarction (MI) during 2 weeks after initiation of clarithromycin treatment, compared to amoxicillin, but this risk was not increased between 2 weeks to 3 years after initiation of antibiotic use [16]. Also, a meta-analysis found an association of macrolide antibiotics and adverse CV outcomes for a short follow-up duration (<30 days), whereas this association was not significant with a longer follow-up duration (>30 days to >3 years) [7]. These data suggest weakening of the adverse CV effects of antibiotics over time.
To date, longitudinal data on the link of antibiotic exposure time in different phases of adulthood with CVD incidence in a population at usual risk are lacking. This study therefore examined associations of duration and life-stages of antibiotic use with CVD risk over 8 years, using detailed information on cumulative antibiotic use during adulthood from the Nurses’ Health Study (NHS).
The NHS is an ongoing cohort study that included 121.701 female registered nurses in the USA in 1976, who were 30-55 years old at enrollment. Information on demographic and lifestyle factors, medical history, and disease status were self-reported. In the current study, baseline data on antibiotic use were obtained from the 2004 questionnaire (n=90.853). In total, 57.726 women reported data on antibiotic use during young (age 20-39 years), middle (age 40-59 years) and late (age >60 years) adulthood. Exclusion was based on history of MI, angina pectoris, stroke and cancer, leaving a study population of 36.429 female participants. Participants were stratified based on self-reported total antibiotic exposure time: short-term use (none, <15 days, or 15 days to 2 months) or long-term use (≥2 months) for each phase of adulthood. Study outcome was incident CVD, defined as a composite of CHD (non-fatal MI or fatal CHD) and total stroke (non-fatal or fatal). Mean follow-up duration was 7.6 years.
Main results
Antibiotic exposure time in different life-stages and risk of CVD
- After adjustment for age, there was a significant association of longer antibiotic exposure time in late (P-trend=0.03) and middle (P-trend=0.001) adulthood and increased risk of CVD, which remained significant after adjustment for covariates (P-trend=0.03 and P-trend<0.001, respectively).
- Higher risk of CVD was seen in those with long-term use in late- (HR: 1.44, 95%CI: 1.13-1.85) or middle (HR: 1.39, 95%CI: 1.04-1.85) adulthood, compared to subject without antibiotic use. After adjustment for covariates, this association remained significant for long-term antibiotic use in late adulthood (HR: 1.32, 95%CI: 1.03-1.70), but not for middle adulthood.
- No significant association of antibiotic use in young adulthood and CVD incidence was observed, compared to those without antibiotics.
Antibiotic exposure time in different life-stages and risk of stroke and CHD
- Antibiotic use for<15 days or 15 days to <2 months during middle adulthood was associated with higher risk of CHD, compared to no antibiotic use in middle adulthood (HR: 1.56, 95%CI: 1.03-2.34 and HR: 1.65, 95%CI: 1.07-2.55, respectively).
- Total exposure of antibiotics for 15 days to <2 months and ≥2 months after age 40 was associated with higher risk of CHD (HR: 2.30 and HR: 2.00, respectively), compared to those without antibiotics. In contrast, there was no significant association between total exposure of antibiotics after age 40 and stroke, compared to no antibiotic usage.
- No significant interactions of antibiotic use with overweight or obesity, dyslipidemia, emphysema or chronic bronchitis, postmenopausal hormone use, or reasons of antibiotic use for respiratory infections on the CVD risk were found.
Conclusion
In this cohort study of women, antibiotic use in middle- (age 40-59 years) and late (age 60+) adulthood was significantly associated with risk of CVD in later life, whereas antibiotic use in young adulthood was not significantly associated with CVD incidence. Antibiotic use in middle adulthood was linked to increased risk of CHD, but not to higher risk of stroke. There may be a link between cumulative antibiotic use during different phases of adulthood and CVD incidence among women aged >60 years.
References
1. Ianiro G, Tilg H, Gasbarrini A. Antibiotics as deep modulators of gut microbiota: between good and evil. Gut 2016;65:1906–1915.
2. Modi SR, Collins JJ, Relman DA. Antibiotics and the gut microbiota. J Clin Invest 2014;124:4212–4218.
3. Reijnders D, Goossens GH, Hermes GD, et al. Effects of gut microbiota manipulation by antibiotics on host metabolism in obese humans: a randomized double-blind placebo-controlled trial. Cell Metab 2016;24:63–74.
4. Jie Z, Xia H, Zhong SL, et al. The gut microbiome in atherosclerotic cardiovascular disease. Nat Commun 2017;8:845.
5. Cheng YJ, Nie XY, Chen XM, et al. The role of macrolide antibiotics in increasing cardiovascular risk. J Am Coll Cardiol 2015; 66:2173–2184.
6. Li X, Wang M, Liu G, et al. Association of macrolides with overall mortality and cardiac death among patients with various infections: a meta-analysis. Eur J Intern Med 2016;28:32–37.
7. Wong AYS, Chan EW, Anand S, et al. Managing cardiovascular risk of macrolides: systematic review and meta-analysis. Drug Saf 2017;40: 663–677.
8. Bin Abdulhak AA, Khan AR, Garbati MA, et al. Azithromycin and risk of cardiovascular death: a meta-analytic review of observational studies. Am J Ther 2015;22:e122–e129.
9. Ray WA, Murray KT, Meredith S, et al. Oral erythromycin and the risk of sudden death from cardiac causes. N Engl J Med 2004;351:1089–1096.
10. Ray WA, Murray KT, Hall K, et al. Azithromycin and the risk of cardiovascular death. N Engl J Med 2012;366:1881–1890.
11. Schembri S, Williamson PA, Short PM, et al. Cardiovascular events after clarithromycin use in lower respiratory tract infections: analysis of two prospective cohort studies. BMJ 2013;346:f1235.
12. Svanstrom H, Pasternak B, Hviid A. Use of azithromycin and death from cardiovascular causes. N Engl J Med 2013;368:1704–1712.
13. Svanstrom H, Pasternak B, Hviid A. Use of clarithromycin and roxithromycin and risk of cardiac death: cohort study. BMJ 2014;349:g4930.
14. Khosropour CM, Capizzi JD, Schafer SD, et al. Lack of association between azithromycin and death from cardiovascular causes. N Engl J Med 2014;370:1961–1962.
15. Chou HW, Wang JL, Chang CH, et al. Risks of cardiac arrhythmia and mortality among patients using new-generation macrolides, fluoroquinolones, and beta-lactam/beta-lactamase inhibitors: a Taiwanese nationwide study. Clin Infect Dis 2015;60:566–577.
16. Wong AY, Root A, Douglas IJ, et al. Cardiovascular outcomes associated with use of clarithromycin: population based study. BMJ 2016;352:h6926.
