High residual inflammatory risk associated with adverse clinical outcomes in patients undergoing PCI with low LDL-c
A single-center prospective PCI-registry showed an independent association of high residual inflammatory risk and adverse clinical outcomes in patients undergoing PCI with LDL-c ≤70 mg/dL at baseline.
Residual Inflammatory Risk in Patients With Low LDL Cholesterol Levels Undergoing Percutaneous Coronary InterventionLiterature - Guedeney P, Claessen BE, Kalkman DN et al. - JACC 2019;73(19):2401-9
Introduction and methods
Patients with coronary artery disease undergoing percutaneous coronary intervention (PCI) show high ischemic risk. One of the strategies to lower adverse events is statin therapy to achieve low-density lipoprotein cholesterol (LDL-c) levels <70 mg/dL [1-3]. However, these patients may also have elevated residual inflammatory risk (RIR) pre- and post-PCI, which is associated with poor prognosis [4,5]. Data on lowering RIR obtained in the CANTOS trial have opened new perspectives in the field of secondary prevention [6,7]. The definition of RIR may be C-reactive protein (CRP) >2 mg/dL, while residual cholesterol risk is mostly defined as LDL-c ≥70 mg/dL [1,2,8].
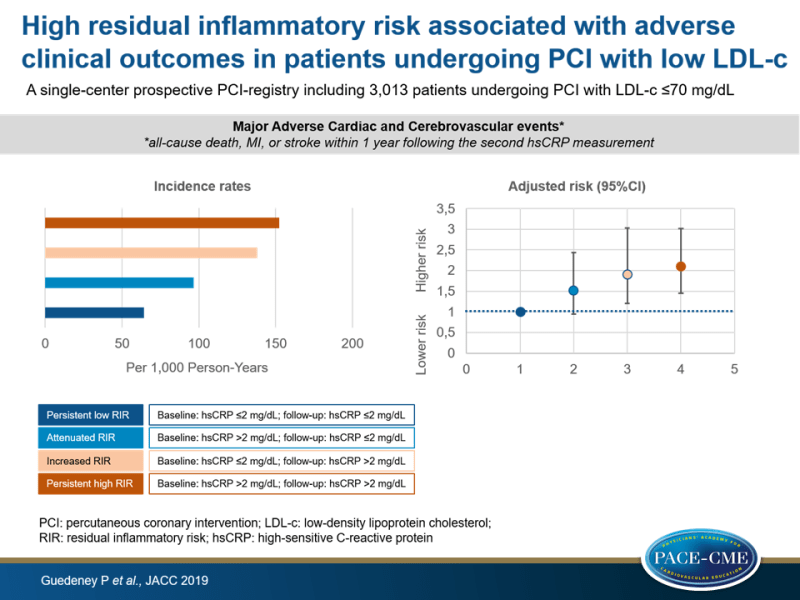
This retrospective analysis characterized the prevalence of persistent high RIR in patients undergoing PCI in a high-volume tertiary care facility with controlled cholesterol risk and evaluated its link with clinical outcomes, using data from the prospective PCI-registry of a large-volume center (The Mount Sinai Hospital, New York, New York). Inclusion was based on PCI between Jan 1, 2009 and Dec 31, 2016, baseline LDL-c ≤70 mg/dL and ≥2 serial high-sensitive CRP (hsCRP) measurements ≥4 weeks apart. High inflammatory status was defined as hsCRP >2 mg/dL. Eligible patients (n= 3,013) were divided into groups based on RIR: persistent high RIR (high inflammatory status at baseline and follow-up), attenuated RIR (first high then low hsCRP), increased RIR (first low then high hsCRP), and persistent low (hsCRP ≤2 mg/dL at baseline and follow-up). The primary endpoint was the composite of major adverse cardiac and cerebrovascular events (MACCE) (all-cause death, MI, or stroke within 1 year following the second hsCRP measurement).
Main results
- Median time between hsCRP measurements was 16 weeks (IQR: 6-66 weeks) for those with persistent high RIR, 19 weeks (6-79 weeks) for those with persistent low RIR, and 16.5 weeks (6-68 weeks) and 35 weeks (7-118 weeks) for those with attenuated and increased RIR, respectively (P<0.001 for overall comparison).
- In the total cohort 34.1% of patients had persistent high RIR, 13.7% attenuated RIR, 11.5% increased RIR, and 40.7% persistent low RIR.
1-Year outcomes according to the residual inflammatory risk
- The highest incidence rate of MACCE was observed in subjects with increased (138.0 per 1,000 PY) or persistent high RIR (152.4 per 1,000 PY), compared to 64.4 per 1,000 PY and 96.6 per 1,000 PY in those with persistent low and attenuated RIR, respectively.
- There was a stepwise increase in incidence rates of MACCE (ranging from 64.4 to 152.4 per 1,000 PY), all-cause death (from 35.9 to 67.3 per 1,000 PY), MI (from 75.5 to 102.4 per 1,000 PY), and the composite outcome of all-cause death, MI, stroke or target vessel vascularization (from 207.7 to 262.6 per 1,000 PY) transitioning from those with persistent low to attenuated, increased and persistent high RIR.
- In multivariable analysis, results remained qualitatively similar, with significantly higher risk of MACCE in those with increased RIR (HR adj: 1.91, 95%CI: 1.21-3.03) and a persistent high RIR (HR adj: 2.10, 95%CI: 1.45-3.02), compared to those with persistent low RIR.
Conclusion
This single-center prospective PCI-registry showed high RIR in one-third of patients undergoing PCI with low LDL-c (≤70 mg/dL) at baseline, which was independently linked to adverse clinical outcomes, indicating the need of more research on inflammation modulating intervention in these patients.
Editorial comment
In his editorial comment, Everett [9] discusses the results obtained by Guedeney et al. that confirm and extend two important findings from previous studies: 1) RIR was observed in one-third of all post-MI patients, even if they have statin therapy or other aggressive LDL-c lowering treatments, and 2) there was an association of RIR and increased risk of MI, stroke and all-cause mortality. These observations suggest an important problem in patients with established coronary artery disease.
Everett explains that risk of MI, stroke or CV death can be reduced with IL-1β inhibition in patients with high RIR, as shown by the CANTOS trial. However, ‘canakinumab is not currently available for this indication in the United States’. In CANTOS, the effect of IL-1β inhibition on clinical outcomes was particularly seen in participants with reduced inflammation, with the greatest benefit found in those who achieved hsCRP <2 mg/dL. Researchers are developing new treatments directed at the NLRP3 inflammasome and its downstream signaling cascade, including IL-1β and IL-6. Everett concludes: ‘Future investigation should focus on identifying safe, efficacious, and affordable treatments for this important pathway of ongoing cardiovascular risk’.
References
1. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/ APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2018 Nov 8 [E-pub ahead of print].
2. Catapano AL, Graham I, De Backer G, et al. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J 2016;37:2999–3058.
3. Boekholdt SM, Hovingh GK, Mora S, et al. Very low levels of atherogenic lipoproteins and the risk for cardiovascular events: a meta-analysis of statin trials. J Am Coll Cardiol 2014;64:485–94.
4. Buffon A, Liuzzo G, Biasucci LM, et al. Preprocedural serum levels of C-reactive protein predict early complications and late restenosis after coronary angioplasty. J Am Coll Cardiol 1999;34:1512–21.
5. Morrow DA, Rifai N, Antman EM, et al. C-reactive protein is a potent predictor of mortality independently of and in combination with troponin T in acute coronary syndromes: a TIMI 11A substudy. Thrombolysis in Myocardial Infarction. J Am Coll Cardiol 1998;31:1460–5.
6. Ridker PM, Everett BM, Thuren T, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med 2017;377: 1119–31.
7. Ibañez B, Fuster V. CANTOS: a gigantic proof of- concept trial. Circ Res 2017;121:1320–2.
8. Ridker PM. Residual inflammatory risk: addressing the obverse side of the atherosclerosis prevention coin. Eur Heart J 2016;37:1720–2.
9. Everett BM. Residual Inflammatory Risk- A Common and Important Risk Factor for Recurrent Cardiovascular Events. JACC 2019;73(19):2410-2
