Non-fasting and fasting lipid levels linked to similar risk of incident CV events
An analysis of the ASCOT-LLA trial showed similar associations of non-fasting and fasting lipid levels with CV events in the same individuals, with high concordance for ASCVD risk categorization based on non-fasting and fasting lipid levels.
Association of Nonfasting vs Fasting Lipid Levels With Risk of Major Coronary Events in the Anglo-Scandinavian Cardiac Outcomes Trial–Lipid Lowering ArmLiterature - Mora S, Chang CL, Moorthy MV et al. - JAMA Intern Med 2019: doi:10.1001/jamainternmed.2019.0392
Introduction and methods
Non-fasting lipids have recently been recommended for routine CV risk assessment [1-8]. These recommendations are based on multiple reports from well-conducted prospective population studies that showed similar CV risk associations for fasting and non-fasting lipid levels [9-13]. In previous studies [1, 9-14] non-fasting and fasting lipid levels were not measured in the same individuals, or a prospective follow-up for comparison of risk for clinical events was lacking when non-fasting and fasting lipid levels were measured in the same individuals. Individual variability in non-fasting and fasting lipid levels may not be reflected in population based studies. Due to this limitation, non-fasting lipid level testing has not been adopted widespread [15,16]. In addition, it is unknown whether non-fasting lipid level testing in CV risk assessment, which is recommended before statin treatment and as part of high blood pressure management, leads to misclassification of risk.
This study (Feb 1, 1998 – Dec 31, 2002) therefore prospectively examined the association of individual fasting and non-fasting lipid levels with prospectively ascertained ASCVD outcomes in 8,270 subjects from the large-scale randomized, double-blinded placebo-controlled clinical Anglo-Scandinavian Cardiac Outcomes Trial–Lipid Lowering Arm (ASCOT-LLA) trial (n=10,305), which investigated risk reduction of incident coronary events with atorvastatine calcium vs. placebo in patients with high risk of ASCVD. Eligible participants were aged 40-79 years, had hypertension and total cholesterol (TC) levels ≤250 mg/dL, were not on statins or fibrates, and had ≥3 additional ASCVD risk factors. As part of the trial protocol fasting and non-fasting lipid levels were measured in the same individual before randomization, with no intervention of advice given between the 2 visits. Non-fasting blood samples were taken approximately 4 weeks before randomization and fasting blood samples during the randomization visit. This study also evaluated possible misclassification of risk with non-fasting instead of fasting lipid levels for subjects that deemed to be eligible for statin treatment based on US or European guidelines. Fasting was defined as no food or drink except for plain water for ≥8 hours before collection of blood samples. Blood samples were analyzed for TC, HDL-c, and triglycerides. The endpoint was major coronary events, defined as non-fatal myocardial infarction (MI) or fatal coronary heart disease. Median follow-up was 3.3 (IQR: 2.8-3.6) years.
Main results
Non-fasting vs. fasting lipid level testing and risk of major coronary events
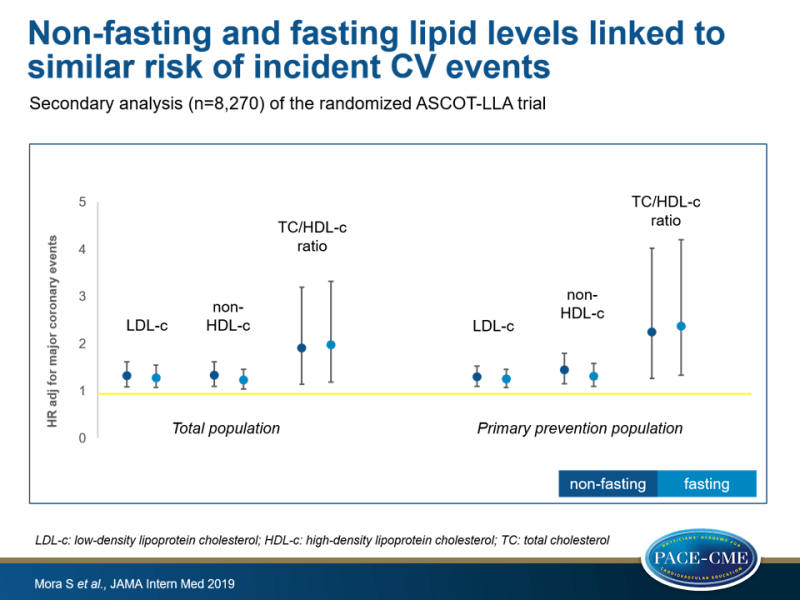
- In the total population, non-fasting and fasting levels of LDL-c (non-fasting HR adj: 1.32, 95%CI: 1.08-1.61, P=0.007 and fasting HR adj: 1.28, 95%CI: 1.07-1.55, P=0.01), non-HDL-c (non-fasting HR adj: 1.33, 95%CI: 1.09-1.61, P=0.004 and fasting HR adj: 1.23, 95%CI: 1.04-1.46, P=0.02), and the ratio of TC to HDL-c (non-fasting HR adj: 1.91, 95%CI: 1.14-3.20, P=0.01 and fasting HR adj: 1.98, 95%CI: 1.18-3.32, P=0.009) were positively associated with risk of major coronary events.
- Non-fasting (HR adj: 0.69, 95%CI: 0.40-1.18, P=0.17) and fasting (HR adj: 0.59, 95%CI: 0.34-1.01, P=0.06) HDL-c levels were non-significantly inversely associated with risk of major coronary events.
- No significant interactions by fasting status for any lipid variable were seen, neither in the total population nor in the primary prevention group.
Non-fasting vs. fasting lipid level testing and CV risk classification
- Classification of participants into categories of ASCVD risk based on non-fasting lipid levels was similar to classification based on fasting lipid levels, whether risk estimation was based on the 2013 ACC/AHA pooled cohort risk equations (94.8% concordance) or the QRISK2 algorithm (98.6% concordance).
- Results among subjects with fasting or non-fasting LDL-c levels 70-189 mg/dL, which is the ACC/AHA range for statin eligibility, were also highly concordant.
- The proportion of reclassification from high-risk to lower-risk categories did not differ between fasting vs. non-fasting lipids for the ACC/AHA guidelines (1.41% vs. 1.40%) or QRISK2 algorithm (0.42% vs. 0.45%).
Conclusion
A secondary analysis of the ASCOT-LLA study showed similar associations of non-fasting and fasting lipid levels with incident major coronary events in the same individuals, with high concordance for CV risk categorization based on non-fasting and fasting lipid levels. These observations are consistent with prior population-based data on fasting and non-fasting lipid levels, which support measurement of non-fasting lipids for routine CV risk assessment and treatment decisions, including initiation of statin treatment.
References
1. Nordestgaard BG, Langsted A, Mora S, et al; European Atherosclerosis Society (EAS) and the European Federation of Clinical Chemistry and Laboratory Medicine (EFLM) Joint Consensus Initiative. Fasting is not routinely required for determination of a lipid profile: clinical and laboratory implications including flagging at desirable concentration cut-points: a joint consensus statement from the European Atherosclerosis Society and European Federation of Clinical Chemistry and Laboratory Medicine. Eur Heart J. 2016;37(25):1944-1958. doi:10.1093/ eurheartj/ehw152
2. Nordestgaard BG, Langsted A, Mora S, et al; European Atherosclerosis Society (EAS) and the European Federation of Clinical Chemistry and Laboratory Medicine (EFLM) Joint Consensus Initiative. Fasting is not routinely required for determination of a lipid profile: clinical and laboratory implications including flagging at desirable concentration cutpoints: a joint consensus statement from the European Atherosclerosis Society and European Federation of Clinical Chemistry and Laboratory Medicine. Clin Chem. 2016;62(7):930-946. doi:10.1373/clinchem. 2016.258897
3. Langlois MR, Chapman MJ, Cobbaert C, et al; European Atherosclerosis Society (EAS) and the European Federation of Clinical Chemistry and Laboratory Medicine (EFLM) Joint Consensus Initiative. Quantifying atherogenic lipoproteins: current and future challenges in the era of personalized medicine and very low concentrations of LDL cholesterol: a Consensus Statement from EAS and EFLM. Clin Chem. 2018;64(7):1006-1033. doi:10.1373/clinchem.2018.287037
4. Leung AA, Nerenberg K, Daskalopoulou SS, et al; CHEP Guidelines Task Force. Hypertension Canada’s 2016 Canadian Hypertension Education Program guidelines for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Can J Cardiol. 2016;32(5):569-588. doi:10.1016/ j.cjca.2016.02.066
5. Anderson TJ, Grégoire J, Pearson GJ, et al. 2016 Canadian Cardiovascular Society guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol. 2016;32(11):1263-1282. doi:10.1016/j.cjca.2016.07.510
6. Nordestgaard BG. A test in context: lipid profile, fasting versus nonfasting. J AmColl Cardiol. 2017;70(13):1637-1646. doi:10.1016/j.jacc. 2017.08.006
7. Farukhi Z, Mora S. The future of low-density lipoprotein cholesterol in an era of nonfasting lipid testing and potent low-density lipoprotein lowering. Circulation. 2018;137(1):20-23. doi:10. 1161/CIRCULATIONAHA.117.031857
8. Gundy SM, Stone NJ, Bailey AL, et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/ APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J AmColl Cardiol. Published online November 3, 2018. doi:10.1016/j.jacc.2018.11.003
9. Di Angelantonio E, Sarwar N, Perry P, et al; Emerging Risk Factors Collaboration. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009;302(18):1993-2000. doi:10.1001/jama.2009. 1619
10. Mora S, Rifai N, Buring JE, Ridker PM. Fasting compared with nonfasting lipids and apolipoproteins for predicting incident cardiovascular events. Circulation. 2008;118(10): 993-1001. doi:10.1161/CIRCULATIONAHA.108.777334
11. Langsted A, Freiberg JJ, Nordestgaard BG. Fasting and nonfasting lipid levels: influence of normal food intake on lipids, lipoproteins, apolipoproteins, and cardiovascular risk prediction. Circulation. 2008;118(20):2047-2056. doi:10.1161/ CIRCULATIONAHA.108.804146
12. Sarwar N, Danesh J, Eiriksdottir G, et al. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation. 2007; 115(4):450-458. doi:10.1161/CIRCULATIONAHA.106. 637793
13. Doran B, Guo Y, Xu J, et al. Prognostic value of fasting versus nonfasting low-density lipoprotein cholesterol levels on long-term mortality: insight from the National Health and Nutrition Examination Survey III (NHANES-III). Circulation. 2014;130(7): 546-553. doi:10.1161/CIRCULATIONAHA.114.010001
14. Mora S. Nonfasting for routine lipid testing: from evidence to action. JAMA Intern Med. 2016;176(7): 1005-1006. doi:10.1001/jamainternmed.2016.1979
15. Driver SL, Martin SS, Gluckman TJ, Clary JM, Blumenthal RS, Stone NJ. Fasting or nonfasting lipid measurements: it depends on the question. J Am Coll Cardiol. 2016;67(10):1227-1234. doi:10.1016/ j.jacc.2015.12.047
16. Rifai N, Young IS, Nordestgaard BG, et al. Nonfasting sample for the determination of routine lipid profile: is it an idea whose time has come? Clin Chem. 2016;62(3):428-435. doi:10.1373/clinchem. 2015.247866
