Blood donor screening as potential strategy for FH screening
In >1 million blood donors, the prevalence of FH was similar to the estimated prevalence of FH in the general population. This suggests that donor screening may represent a new approach for FH screening and intervention.
Identifying Familial Hypercholesterolemia Using a Blood Donor Screening Program With More Than 1 Million Volunteer DonorsLiterature - Jackson CL, Keeton JZ, Eason SJ et al. - JAMA Cardiol 2019: doi:10.1001/jamacardio.2019.1518
Introduction and methods
Familial hypercholesterolemia (FH) remains underdiagnosed and undertreated in the general population [1,2]. It is crucial to diagnose FH and start cholesterol-lowering therapy in order to reduce the associated risk of coronary artery disease (CAD) [3,4]. A coordinated FH screening system is currently lacking in the US [5,6]. Blood donation may play a role in FH screening. Beyond assessing transmissible infections, it is also possible to examine non-infectious conditions or risks with donor screening[7]. For instance, total cholesterol (TC) can already be tested in many blood donor centers at no charge [8] and glycated hemoglobin to screen for diabetes [9,10].
This study therefore estimated the prevalence of FH in the Carter BloodCare database including more than 1 million blood donors as a preliminary step in investigating blood donation as a strategy for FH screening and intervention. Eligible blood donors were persons ≥16 years of age who voluntarily donated blood to Carter BloodCare between Jan 2002 and Dec 2016. In each blood sample TC was measured. FH was classified using the Make Early Diagnosis to Prevent Early Death (MEDPED) criteria [11], with TC thresholds of 270, 290, 340, and 260 mg/dL for those aged <20 years, 20-29 years, 30-39 years, and ≥40 years, respectively. The maximum TC value was used for individuals with more than one blood donation.
Main results
- This study included 3,0382,420 blood donations from 1,178,102 donors. The median number of blood donations was 1 (IQR: 1-3). The median TC level was 183 (IQR: 157-212) mg/dL.
Prevalence of FH in blood donors
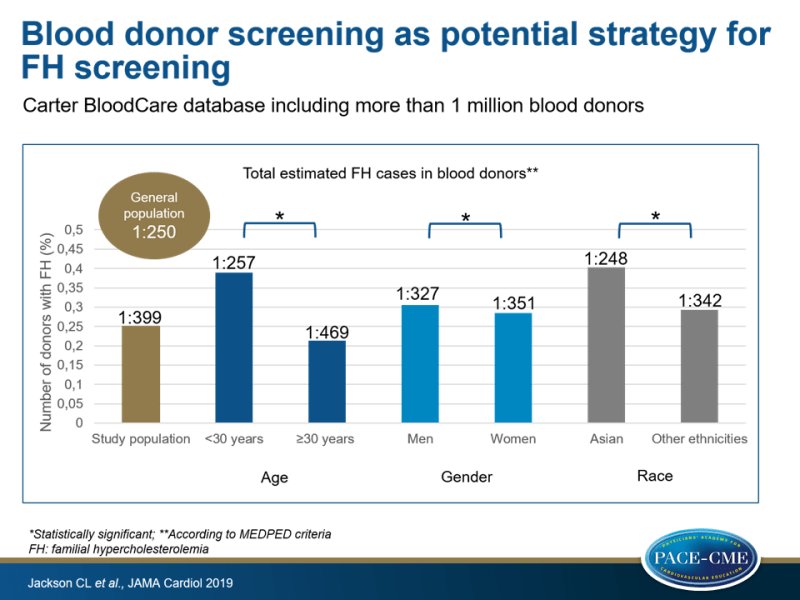
- 3,473 FH cases were found according to MEDPED criteria (prevalence 1:399 donors).
- A greater prevalence of FH was observed in donors aged <30 years (1:257 [2,127 of 546,619]) vs. participants aged ≥30 years (1:469 [1,346 of 631,483]) (P<0.001) and in men (1:327 [1,708 of 558,462]) vs. women (1:351 [1,765 of 619,583]) (P=0.03).
- The prevalence did not significantly differ between groups based on race, except that Asian subjects were more likely to have FH (1:248 [128 of 31,773]) compared to donors of all other ethnicities (1:342 [3,345 of 1,146,329]) (P<0.001).
Persistence of meeting FH criteria over multiple donations
- Among those who met FH criteria, 1,254 (36.1%) individuals donated once, and 2,219 (63.9%) participants did multiple donations.
- Among those with repeated blood donations who met FH criteria at least once, 3,116 of their 10,833 (28.8%) donations met FH criteria. This included 779 of 1,629 (47.8%) donations meeting less stringent MEDPED TC criteria (TC >270 mg/dL; age <20 years), and 954 of 4,808 (19.8%) donations meeting the most stringent criteria (TC >360 mg/dL; age >40 years).
- Among donors meeting the most stringent criteria, a larger proportion of repeated TC values were close to normal levels (TC <210 mg/dL) (1,508 of 4,808 [31.4%] vs. 276 of 1,629 [16.9%]).
- Among subjects with repeated blood donations who met FH criteria only once, the median difference between maximum and minimum TC levels was 109 (IQR: 62-177) mg/dL (a 33% difference) vs. 28 (IQR: 14-47) mg/dL (a 14% difference) in those with repeated blood donations who never met FH criteria.
Conclusion
In this large study with volunteer blood donors, the estimated prevalence of FH according to MEDPED criteria was similar to the US population estimate of 1:250. Blood donor screening might therefore represent a novel and potentially cost-effective strategy to identify cases of FH, especially in younger subjects who are not engaged in the medical system. Also, blood donor screening may be a strategy to guide cascade screening.
Editorial comment
In his editorial comment [12], Stephen R Daniels highlights results obtained by Jackson et al. and discusses two issues related to effective screening for and treatment for FH. The first issue concerns repeated blood donations in donors who initially were classified as having FH but who met criteria for FH only 29% of the time. TC levels might vary in time, which would mean that some initial measurements may be false positives. The variability may also indicate that some of those participants later received treatment. However, data to answer these questions were not available in the database.
Secondly, Daniels explains that a connection of the screening program to the health care system, in this case the source of primary care for blood donors, is essential for the screening program to be effective. Patients and their health care professionals should understand and interpret cholesterol levels correctly. Measuring cholesterol levels may not be the main issue in our current health system. Daniels emphasizes that, in fact, translation of information on cholesterol levels into effective therapy and optimum adherence may be the biggest barrier for an effective blood screening program.
Daniels emphasizes that improvement of our approach to screening and treatment for FH is highly needed. “Given the increasing use of electronic health data, it is possible that data from blood donations and other settings, such as health screening, could be integrated into a broadly and more useable health record that could result in improved treatment for familial hypercholesterolemia. More work will be needed to establish such a comprehensive system.”
References
1. Nordestgaard BG, Chapman MJ, Humphries SE, et al; European Atherosclerosis Society Consensus Panel. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: consensus statement of the European Atherosclerosis Society. Eur Heart J. 2013;34(45):3478-90a. doi:10.1093/eurheartj/eht273
2. deGoma EM, Ahmad ZS, O’Brien EC, et al. Treatment gaps in adults with heterozygous familial hypercholesterolemia in the United States: data from the CASCADE-FH registry. Circ Cardiovasc Genet. 2016;9(3):240-249. doi:10.1161/CIRCGENETICS.116. 001381
3. Umans-Eckenhausen MA, Defesche JC, Sijbrands EJ, et al. Review of first 5 years of screening for familial hypercholesterolaemia in the Netherlands. Lancet. 2001;357(9251):165-168. doi:10.1016/S0140-6736 (00)03587-X
4. Knowles JW, Rader DJ, KhouryMJ. Cascade screening for familial hypercholesterolemia and the use of genetic testing. JAMA. 2017;318(4):381-382. doi:10.1001/jama.2017.8543
5. Safarova MS, Liu H, Kullo IJ. Rapid identification of familial hypercholesterolemia from electronic health records: the SEARCH study. J Clin Lipidol. 2016;10(5):1230-1239. doi:10.1016/j.jacl.2016.08.001
6. Wald DS, Bestwick JP, Morris JK, et al. Child-parent familial hypercholesterolemia screening in primary care. N Engl J Med. 2016;375(17):1628-1637. doi:10.1056/ NEJMoa1602777
7. Shaz BH, Kessler D, Hillyer CD. Evaluating the role of blood collection centers in public health: a status report. Transfus Med Rev. 2012;26(1):58-67. doi:10.1016/j.tmrv.2011.07.002
8. Eason S, Goudar S, Centilli J, et al. Experience with routine total nonfasting blood cholesterol screening of volunteer blood and component donors. Transfusion. 2011;51(4):731-736. doi:10.1111/j.1537-2995.2010.02920.x
9. Gore MO, Eason SJ, Ayers CR, et al. Glycated hemoglobin in 14,850 adolescent blood donors: a pilot screening program. Diabetes Care. 2014;37 (1):e3-e4. doi:10.2337/dc13-0908
10. Gore MO, Eason SJ, Ayers CR, et al. High prevalence of elevated haemoglobin A1C among adolescent blood donors: results from a voluntary screening programme including 31,546 adolescents. Diab Vasc Dis Res. 2015;12(4):272-278. doi:10.1177/1479164115579799
11. Williams RR, Hunt SC, Schumacher MC, et al. Diagnosing heterozygous familial hypercholesterolemia using new practical criteria validated by molecular genetics. Am J Cardiol. 1993; 72(2):171-176. doi:10.1016/0002-9149(93)90155-612. Daniels SR. Screening for Familial Hypercholesterolemia. JAMA Cardiol 2019.: doi:10.1001/jamacardio.2019.1509
