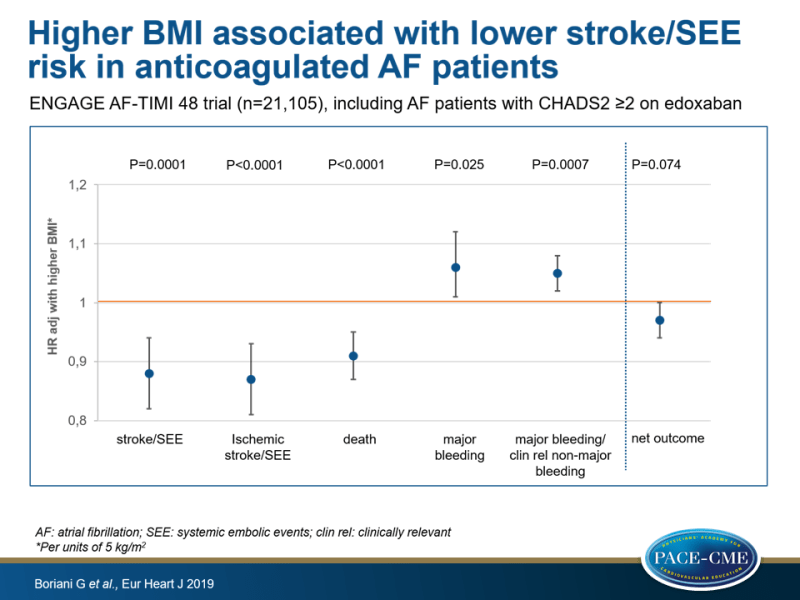
Higher BMI associated with lower stroke/SEE risk in anticoagulated AF patients
ENGAGE AF-TIMI 48 data show that BMI was negatively associated with risk of stroke/SEE and positively associated with risk of bleeding, although sex differences were seen.
Relationship between body mass index and outcomes in patients with atrial fibrillation treated with edoxaban or warfarin in the ENGAGE AF-TIMI 48 trialLiterature - Boriani G, Ruff CT, Kuder JF et al., - Eur Heart J. 2019. 40(19) : 1541-1550. https://doi.org/10.1093/eurheartj/ehy861
Introduction and methods
The incidence of atrial fibrillation (AF) is higher in obese persons than in non-obese persons [1]. A retrospective analysis of AFFIRM data, however, suggested that survival of patients was better in obese patients with AF [2]. BMI is not considered a major risk factor for stroke or bleeding in patients with AF [3]. In other patient groups and the general population, however, higher BMI is associated with worse outcomes [4-6]. A higher bleeding risk in patients with lower BMI has also been reported for patients with atherothrombotic disease who receive antiplatelet therapy [7].
This study investigated the relationship between BMI and pharmacokinetic, pharmacodynamic and clinical outcomes in patients enrolled in the ENGAGE AF-TIMI 48 trial [8,9]. This was a randomized trial that evaluated two dose regimens of the factor Xa remmer edoxaban (higher dose [HDE]: 60 mg once daily, and lower dose [LDE]: 30 mg once daily) compared with warfarin (INR 2.0-3.0). Edoxaban doses were halved in case of estimated creatinine clearance of ≤50 mL per minute, body weight of ≤60 kg, or the concomitant use of verapamil, quinidine, or dronedarone. Only HDE results are presented, as this is the only edoxaban dose that has been approved for clinical use. Median follow-up in the ENGAGE AF-TIMI 48 trial was 2.8 years. 21,105 Patients who had AF documented in the year preceding randomization with CHADS2 score ≥2 were included. The primary efficacy endpoint was the composite of adjudicated stroke or systemic embolic events (SEE) (ITT analysis) and the principal safety outcome was adjudicated ISTH major bleeding in the safety population while on treatment.
Main results
- 0.8% of 21,105 patients with BMI information available were underweight (BMI<18.5), 21.4% normal (18.5 to <25), 37.6% overweight (25 to <30), 24.8% moderately obese (30 to <35) and 10.0% were severely obese (35 to <40) and 5.5% were very severely obese (≥40).
- Trough edoxaban plasma concentrations measured 1 month after randomization did not differ between BMI categories, nor did anti-Factor Xa activity levels at trough.
- When considering BMI as a continuous variable (in units of 5 kg/m² increase) in the whole cohort, higher BMI was significantly and independently associated with lower risks of stroke/SEE (HR: 0.88, 95%CI: 0.82-0.94, P=0.0001). Risks of ischemic stroke/SEE (HR: 0.87, 95%CI: 0.81-0.93, P<0.0001) and death (HR: 0.91, 95%CI: 0.87-0.95, P=0.0001) were also lower with increasing BMI.
- Higher BMI was independently associated with a higher risk of major bleeding (HR: 1.06, 95%CI: 1.01-1.12, P=0.025) and of major or clinically relevant non-major bleeding (HR: 1.05, 95%CI: 1.02-1.08, P=0.0007).
- Net outcome (composite of stroke, SEE, major bleeding or death) did not differ across BMI categories (P trend=0.44).
- An interaction between sex and the relation between BMI and ischemic stroke/SEE was seen, such that men showed a lower risk with increasing BMI, while women did not. Similarly, the higher risk of major or clinically relevant non-major bleeding with increasing BMI in women was not observed in men.
Conclusion
This analysis of ENGAGE AF-TIMI 48 trial data in patients with AF shows that over 40% of the population were obese. Higher BMI was independently associated with lower adjusted risks of stroke/SEE and of death and with higher risk of bleeding. Net clinical outcome was comparable between higher and normal BMI categories. Sex differences were noted, such that in men, the risk of stroke/SEE declined with higher BMI, but not in women, and in women only, an increasing trend in risk of bleeding was seen with BMI.
References
1. Wang TJ, Parise H, Levy D, et al. Obesity and the risk of new-onset atrial fibrillation. JAMA 2004;292:2471–2477.
2. Badheka AO, Rathod A, Kizilbash MA, et al. Influence of obesity on outcomes in atrial fibrillation: yet another obesity paradox. Am J Med 2010;123:646–651.
3. Lip GY, Lane DA. Stroke prevention in atrial fibrillation: a systematic review. JAMA 2015;313:1950–1962.
4. Kurth T, Gaziano JM, Berger K, et al. Body mass index and the risk of stroke in men. Arch Intern Med 2002; 162:2557–2562.
5. Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009;373: 1083–1096.
6. Twig G, Yaniv G, Levine H, et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N Engl J Med 2016;374: 2430–2440.
7. Mak KH, Bhatt DL, Shao M, et al. The influence of body mass index on mortality and bleeding among patients with or at high-risk of atherothrombotic disease. Eur Heart J 2009;30:857–865.
8. Ruff CT, Giugliano RP, Antman EM et al. Evaluation of the novel factor Xa inhibitor edoxaban compared with warfarin in patients with atrial fibrillation: design and rationale for the Effective aNticoaGulation with factor xA next Generation in Atrial Fibrillation-Thrombolysis In Myocardial Infarction study 48 (ENGAGE AF-TIMI 48). Am Heart J 2010;160:635–641.
9. Giugliano RP, Ruff CT, Braunwald E, et al; ENGAGE AF-TIMI 48 Investigators. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med 2013;369:2093–2104.
