Systolic and diastolic hypertension independently associated with CV outcomes
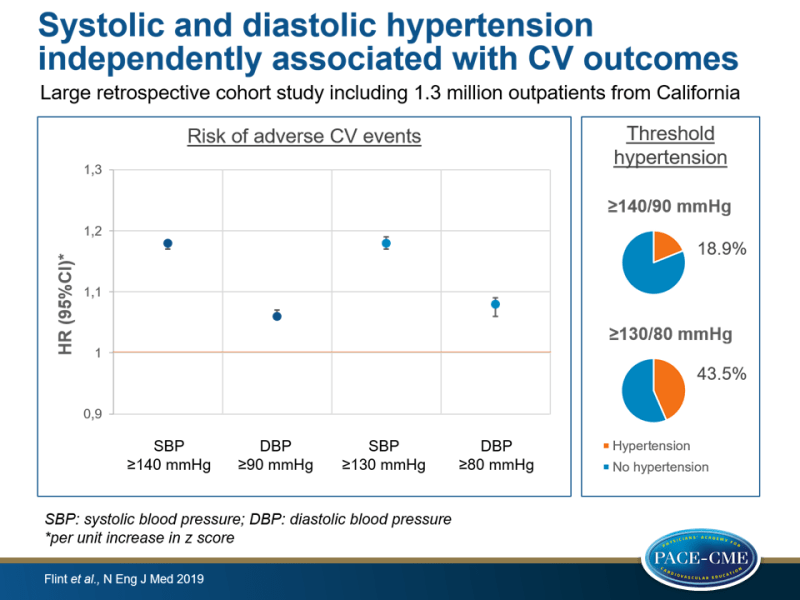
In a large cohort study of 1.3 million participants, both systolic and diastolic hypertension were associated with composite of MI, ischemic stroke and hemorrhagic stroke, independent of thresholds defining hypertension.
Effect of Systolic and Diastolic Blood Pressure on Cardiovascular OutcomesLiterature - Flint AC, Conell C, Ren X, et al. - N Engl J Med 2019;381:243-51. doi: 10.1056/NEJMoa1803180
Introduction and methods
Focus has been on systolic hypertension after the Framingham Heart Study and other studies demonstrated that systolic hypertension is more important as a predictor of CV outcomes [1]. This was reflected in the 2000 clinical advisory statement from the National High Blood Pressure Education Program [2] and the American College of Cardiology (ACC)–American Heart Association (AHA) risk estimation tool [3] does not include diastolic blood pressure (DBP) for determination of CV risk. In contrast to this, clinicians still record and target values for both systolic BP (SBP) and DBP.
The threshold to define hypertension in the 2017 US hypertension guidelines has changed to 130/80 mm Hg [4], whereas in the European guidelines the threshold is still 140/90 mmHg. Lower targets in the new US hypertension guidelines might result in more patients with diastolic hypotension [6,7,9,10], which might be of concern due to a possible J-curve relationship between DBP and adverse outcomes [5-9].
This study examined whether SBP and DBP were independently associated with the risk of adverse CV outcomes. In addition, the effect of the threshold for the definition of hypertension on the association between SBP and DBP with outcomes was assessed, and a possible J-curve relationship between DBP and outcomes was explored.
A retrospective cohort study was conducted analyzing data from outpatients from Kaiser Permanente Northern California (KPNC), a large integrated health care system [11]. During a 2-year baseline period, initial BP measurements and coexisting conditions were recorded and over an 8-year observation period, additional BP measurements were performed and occurence of MI, ischemic stroke or hemorrhagic stroke was documented. A total of 1.3 million study participants were enrolled, who were ≥18 years and had one BP measurement at baseline (Jan 2007-Dec 2008) and ≥2 BP-measurements during the observation period (Jan 2009-Dec 2016). BP was measured using an automated oscillometric BP cuff.
To determine average hypertension burdens above the thresholds defining hypertension (≥140/90 mmHg or ≥130/80 mmHg), measures were zeroed at the threshold for values at or below the threshold and values above the threshold were expressed in mmHg. Therefore, hypertension burdens were continuous variables with zero values for normal or low BP, and values were standardized to z scores (± SDs from the mean).
Main results
- Median number of BP measurements per participant was 22 (IQR: 13-36).
- Applying the 140/90 mmHg threshold resulted in 18.9% of participants with hypertension, and for 130/80 mmHg this was 43.5%.
- Relationship between DBP and composite outcome showed a J-shaped curve, with increased risk in both lowest and highest deciles for DBP. Compared to middle two quartiles, HR for those in the lowest quartile of DBP was 1.44 (95%CI:1.41-1.48), after full adjustment HR was 0.90 (95CI:0.88-0.92) and after adjustment without control for age HR was 1.15 (95%CI:1.13-1.18), indicating that age partially explained the relationship.
- Burden of systolic hypertension (≥ 140 mm Hg) was associated with increased risk of composite outcome (HR per unit increase in z score: 1.18, 95%CI:1.17-1.18, P<0.001). Burden of diastolic hypertension (≥ 90 mmHg) was also independently associated with composite outcome (HR per unit increase in z score: 1.06; 95%CI:1.06-1.07, P<0.001).
- Similar results were shown with thresholds of 130/80 mmHg. For SBP ≥130 mmHg, HR per unit increase in z score was 1.18 (95%CI:1.17-1.19, P<0.001, and for DBP ≥80 mmHg, HR was 1.08, 95%CI:1.06-1.09, P<0.001).
- In participants with SBP <140 mmHg, diastolic hypertension burden >90 mmHg was associated with increased risk for composite outcome (HR per unit increase in z score: 1.66, 95%CI:1.53-1.79, P<0.001) and also in those with SBP <130 mmHg, diastolic hypertension burden >80 mmHg was associated with adverse outcomes (HR per unit increase in z score: 1.52, 95%CI: 1.03-2.23, P=0.03).
- Systolic hypertension ≥140 mm Hg had a greater effect on adverse outcomes in those in the lowest quartile of DBP (HR per unit increase in z score: 1.21, 95%CI:1.20-1.23, P<0.001) than in those in the highest quartile of DBP (HR: 1.16, 95%CI:1.15-1.17, P<0.001). Similar results were observed when a threshold for defining systolic hypertension of ≥ 130 mm Hg was used.
Conclusion
This large retrospective cohort study including people from Northern California demonstrated that both systolic and diastolic hypertension were associated with increased risk for adverse CV outcomes. The association was similar when using threshold defining hypertension as ≥140/90 mmHg or ≥130/80 mmHg. A J-curve relationship between DBP and outcomes was seen, with higher risk in those with lowest and highest DBP values. The higher risk of outcomes in those with lower DBP could partially be explained by age, other covariates and by a greater effect of systolic hypertension.
References
1. Kannel WB, Dawber TR, McGee DL. Perspectives on systolic hypertension: the Framingham Study. Circulation 1980; 61:1179-82.
2. Izzo JL Jr, Levy D, Black HR. Clinical advisory statement: importance of systolic blood pressure in older Americans. Hypertension 2000; 35: 1021-4.
3. Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014; 63: 2935-59.
4. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018; 71(6): e13-e115.
5. Bhatt DL. Troponin and the J-curve of diastolic blood pressure: when lower is not better. J Am Coll Cardiol 2016; 68: 1723-6.
6. Rahman F, McEvoy JW. The J-shaped curve for blood pressure and cardiovascular disease risk: historical context and recent updates. Curr Atheroscler Rep 2017; 19: 34.
7. Vidal-Petiot E, Greenlaw N, Ford I, et al. Relationships between components of blood pressure and cardiovascular events in patients with stable coronary artery disease and hypertension. Hypertension 2018; 71: 168-76.
8. Vidal-Petiot E, Ford I, Greenlaw N, et al. Cardiovascular event rates and mortality according to achieved systolic and diastolic blood pressure in patients with stable coronary artery disease: an international cohort study. Lancet 2016; 388: 2142-52.
9. McEvoy JW, Chen Y, Rawlings A, et al. Diastolic blood pressure, subclinical myocardial damage, and cardiac events: implications for blood pressure control. J Am Coll Cardiol 2016; 68: 1713-22.
10. Beddhu S, Chertow GM, Cheung AK, et al. Influence of baseline diastolic blood pressure on effects of intensive compared with standard blood pressure control. Circulation 2018; 137: 134-43.
11. Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001; 285: 2370-5.
