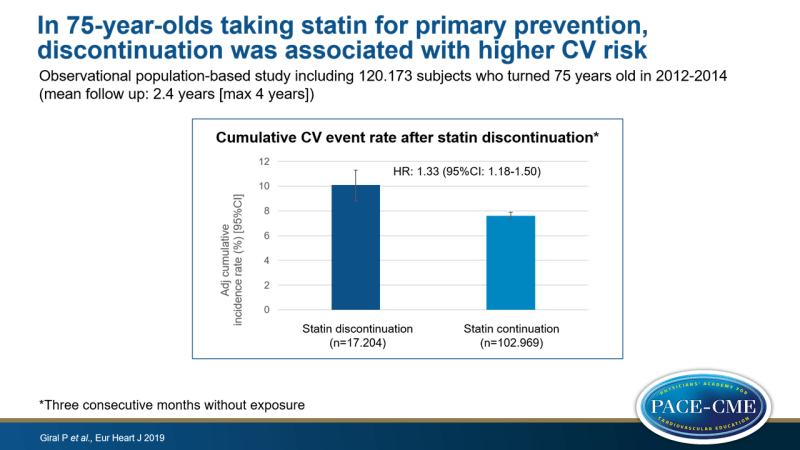
In 75-year-olds taking statin for primary prevention, discontinuation was associated with higher CV risk
Observational population-based study suggests that continuing statin therapy after the age of 75 years may reduce CV risk in persons taking the medication for primary prevention.
Cardiovascular effect of discontinuing statins for primary prevention at the age of 75 years: a nationwide population-based cohort study in FranceLiterature - Giral P, Neumann A, Will A et al., - Eur Heart J 2019, ehz458, https://doi.org/10.1093/eurheartj/ehz458
Introduction and methods
The use of statin therapy in primary prevention in the elderly is topic of debate, and little evidence is available for or against its benefit [1-4]. Both the European guidelines on the management of dyslipidemias and the one on CV disease prevention in clinical practice, give no recommendation for or against statin use for primary prevention in individuals over the age of 75 years [5,6]. The American 2018 ACC/AHA guidelines only recommend a shared decision-making process between clinician and patient and regular reassessment. The ACC/AHA guidelines do mention that if CAC score is 0, the likelihood of benefits does not outweigh the risks in older adults [7].
An outstanding question for clinical practice is whether existing statin therapy can be stopped in older people without a history of CV disease. This study therefore aimed to assess the effect of statin discontinuation on CV outcomes in persons who turned 75 years old in 2012-2014, who were previously adherent to statin therapy (medication possession ratio [MPR] >80%) for at least two years with no history of CV disease. This retrospective study used French healthcare databases. Individuals with a diagnosis of CV disease or a related in-hospital procedure in the previous 2 years and patients taking combined use of CV preventive medication or long-term treatment with an antiplatelet agent other than aspirin, were excluded. Statin therapy was considered to be discontinued if a person presented three consecutive months without exposure. The outcome of interest was hospital admission for a CVD event. 102.173 patients were included and mean follow-up was 2.4 years (max: 4 years). The total follow-up of 3.067.730 months included 176.373 (5.7%) patient-months after statin discontinuation.
Main results
- 5396 Patients were admitted for CV events (crude incidence rate: 2.1 per 100 patient-years), among which 2299 with a coronary events and 2328 patients with a cerebrovascular event, and 769 other patients with another vascular event. 3243 Patients died during follow-up.
- Factors related to statin discontinuation included hospital admission during follow-up (adjOR: up to 3.28), admission to a skilled nursing home (adjOR: 2.66), metastatic solid tumor (adjOR: 2.22) and initiation of enteral or oral feeding (aOR: 2.13).
- Discontinuation of most other CV drugs was associated with higher probability of statin discontinuation, while initiation or continuation of baseline use decreases this probability.
- 17.204 patients discontinued statin therapy during follow-up, of whom 7.336 (42.6%) resumed therapy.
- The adjHR for admission for a CV event in those who discontinued vs. those wo continued using statins was 1.33 (95%CI: 1.18-1.50). Four years after the 75th birthday, the adjusted cumulative incidence rates were 10.1% and 7.6%, respectively.
- AdjHR for admissions for coronary, cerebrovascular and other vascular events were 1.46 (95%CI: 1.21 – 1.75), 1.26 (95%CI: 1.05-1.51) and 1.02 (95%CI: 0.74-1.40), respectively.
Conclusion
In a population-based primary prevention cohort of 75-year-old individuals who were previously adherent to statin therapy for at least 2 years, discontinuation of statins was associated with a higher risk of admission for a CV event. The association with admission was stronger for coronary events than for cerebrovascular events. Considering the observational nature of these data, the findings should be confirmed in randomized studies.
References
1. Strandberg TE, Kolehmainen L, Vuorio A. Evaluation and treatment of older patients with hypercholesterolemia: a clinical review. JAMA 2014;312:1136–1144.
2. Petersen LK, Christensen K, Kragstrup J. Lipid-lowering treatment to the end? A review of observational studies and RCTs on cholesterol and mortality in 80þ-year olds. Age Ageing 2010;39:674–680.
3. Gurwitz JH, Go AS, Fortmann SP. Statins for primary prevention in older adults: uncertainty and the need for more evidence. JAMA 2016;316:1971–1972.
4. Pedro-Botet J, Climent E, Chillaro´n JJ, et al. Statins for primary cardiovascular prevention in the elderly. J Geriatr Cardiol 2015;12: 431–438.
5. Catapano AL, Graham I, De Backer G, et al; ESC Scientific Document Group. 2016 ESC/EAS Guidelines for the management of dyslipidaemias. Eur Heart J 2016;37:2999–3058.
6. Piepoli MF, Hoes AW, Agewall S, et al; ESC Scientific Document Group. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016;37: 2315–2381.
7. Grundy SM, Stone NJ, Bailey AL, et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol. Circulation 2018;2018:CIR0000000000000625.
