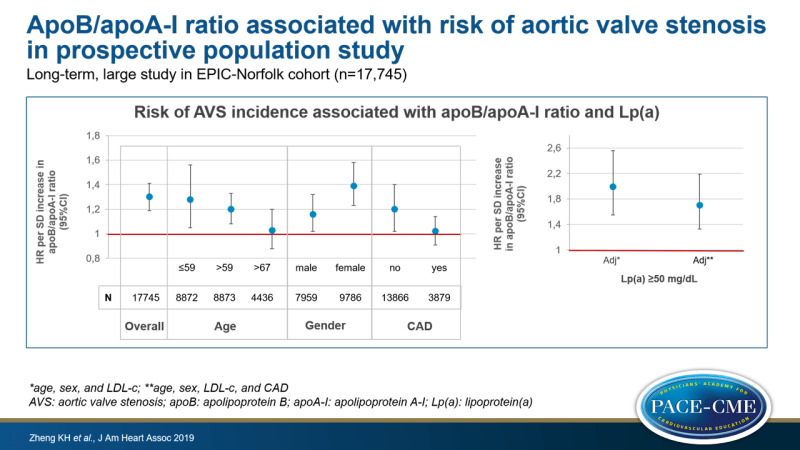
ApoB/apoA-I ratio associated with risk of aortic valve stenosis in prospective population study
Long-term, large study in EPIC-Norfolk cohort finds association of apoB/apoA-I ratio with the risk of aortic valve stenosis incidence, and shows that lp(a) is an independent risk factor for AVS.
apoB/apoA-I Ratio and Lp(a) Associations With Aortic Valve Stenosis Incidence: Insights From the EPIC-Norfolk Prospective Population StudyLiterature - Zheng KH, Arsenault BJ, Kaiser Y et al., - J Am Heart Assoc. 2019;8(16):e013020
Introduction and methods
The involvement of the atherogenic apolipoprotein B (apoB)-containing lipoproteins, such as LDL-c and lipoprotein (a) [lp(a)], in the pathogenesis of aortic valve stenosis (AVS) is well established [1,2]. Trials evaluating lowering LDL-c have, however, failed to show a favorable impact on AVS progression [3]. No Lp(a)-lowering trials have been conducted yet. Thus, there is currently no proven medical therapy to reduce disease progression of AVS.
The apoB/apolipoprotein A-I (apoA-I) ratio and Lp(a) have been described to be associated with future AVS surgery, only in patients with concomitant coronary artery disease (CAD), and not in those with ‘isolated AVS’ [4]. This suggests that different phenotypes of AVS exist, and different pathogenic mechanisms and risk factors may be involved. Other data have suggested that lipoprotein-mediated pathology may be dominant in younger patients, while other risk factors may be more relevant to disease progression in older patients [5]. Risk factors for AVS incidence and progression may also vary due to different pathophysiological processes depending on the stage of disease [6].
This study set out to assess the associations between apoB/apoA-I ratio, Lp(a) and AVS incidence in a prospective, longitudinal study (EPIC-Norfolk, 25,639 participants [7]). Moreover, it was assessed how clinical characteristics modify these associations. Complete data were available for 17,745 participants. 579 Participants reported a history of CAD at baseline and 3300 had a CAD incident during follow-up. After a median follow-up of 19.8 years, 403 (2.2%) incident AVS cases were noted.
Main results
- Cases had higher apoB/apoA-I ratio than controls (0.70±0.19 vs. 0.64±0.19, P<0.001).
- The unadjusted HR for AVS risk was 1.30 (95%CI: 1.19-1.41) per SD increase in the ratio. After adjustment for age and sex, a weaker association was seen (HR: 1.18, 95%CI: 1.07-1.30, P=0.001). After additional adjustment for concomitant CAD, the association was no longer statistically significant (HR: 1.06, 95%CI: 0.97-1.17, P=0.215).
- When stratifying the data by age, younger participants (<59 years) showed a somewhat higher risk for AVS for each SD increase in apoB/ApoA-I (HR: 1.28, 95%CI: 1.05-1.56, P=0.014) than older participants (>59 years, HR: 1.20, 95%CI: 1.08-1.33, P=0.001). In those older than 67 years, the ratio was not associated with AVS risk (HR: 1.03, 95%CI: 0.88-1.20, P=0.74).
- When stratifying for sex, a stronger association for the ratio and AVS risk was seen in women (HR: 1.39, 95%CI: 1.23-1.58) than in men (HR: 1.16, 95%CI: 1.02-1.32, P=0.25).
- When stratifying for CAD, those without concomitant CAD showed a significant association between the ratio and AVS risk (HR: 1.20, 95%CI: 1.02-1.40, P=0.025), but those with CAD did not (HR: 1.02, 95%CI: 0.91-1.14, P=0.78).
- The previously reported independent association between elevated Lp(a) levels (≥50 mg/dL) and risk of incident AVS (adjusted for age, sex and LDL-c, HR: 1.99, 95%CI: 1.55-2.56, P<0.001), was not markedly changed by additional adjustment for concomitant CAD (HR: 1.70, 95%CI: 1.33-2.19, P<0.001).
Conclusion
As a measure that reflects the balance between atherogenic apoB-containing particles and antiatherogenic HDL particles, the apoB/apoA-I ratio captures both dyslipidemia and dysmetabolic regulation. In the EPIC-Norfolk population study, the ratio was a strong predictor of AVS incidence, especially in younger and female participants. This supports the hypothesis that lipoproteins are involved in the pathogenesis of AVS. Lp(a) was an independent risk factor for AVS incidence.
References
1. Smith JG, Luk K, Schulz CA, et al; Cohorts for Heart and Aging Research in Genetic Epidemiology Extracoronary Calcium Working Group. Association of low-density lipoprotein cholesterol-related genetic variants with aortic valve calcium and incident aortic stenosis. JAMA. 2014;312: 1764–1771.
2. Thanassoulis G, Campbell CY, Owens DS, et al.; CHARGE Extracoronary Calcium Working Group. Genetic associations with valvular calcification and aortic stenosis. N Engl J Med. 2013;368:503–512.
3. Zhao Y, Nicoll R, He YH, Henein MY. The effect of statins on valve function and calcification in aortic stenosis: a meta-analysis. Atherosclerosis. 2016;246: 318–324.
4. Ljungberg J, Holmgren A, Bergdahl IA, et al. Lipoprotein(a) and the apolipoprotein B/A1 ratio independently associate with surgery for aortic stenosis only in patients with concomitant coronary artery disease. J Am Heart Assoc. 2017;6:e007160. DOI: 10.1161/JAHA.117.007160
5. Tastet L, Capoulade R, Shen M, et al. ApoB/ApoA-I ratio is associated with faster hemodynamic progression of aortic stenosis: results from the PROGRESSA (metabolic determinants of the progression of aortic stenosis) study. J Am Heart Assoc. 2018;7:e007980. DOI: 10.1161/JAHA.117.007980
6. Pawade TA, Newby DE, Dweck MR. Calcification in aortic stenosis: the skeleton key. J Am Coll Cardiol. 2015;66:561–577.
7. Day N, Oakes S, Luben R, et al. EPICNorfolk: study design and characteristics of the cohort. European Prospective Investigation of Cancer. Br J Cancer. 1999;80(suppl 1):95–103.
