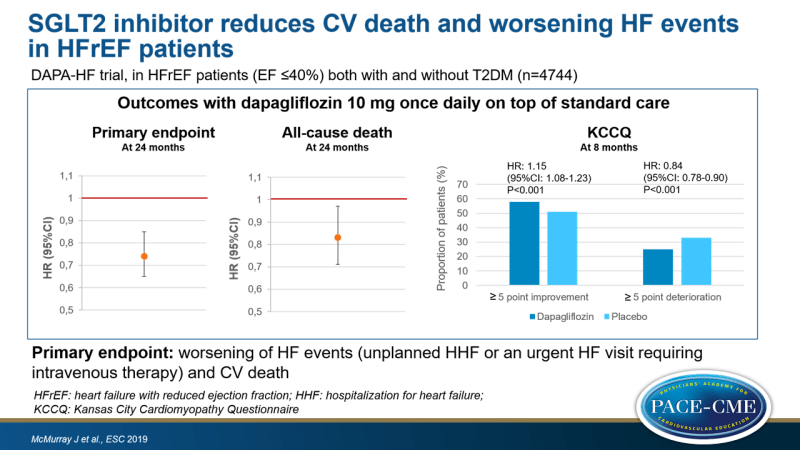
SGLT2 inhibitor reduces CV death and worsening HF events in HFrEF patients
ESC 2019 In HFrEF patients with and without diabetes, dapagliflozin therapy reduced the composite of CV death and worsening HF events compared to placebo.
Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction (DAPA-HF)News - Sep. 1, 2019
Presented at the ESC congress 2019 in Paris, France by: John McMurray (Glasgow, UK)
Introduction and methods
In large CV outcome trials, sodium-glucose co-transporter 2 (SGLT2) inhibitors reduced the development of heart failure (HF) in patients with type 2 diabetes (T2DM). It is however unknown whether SGLT2 inhibitors can be used to treat patients with HF. In addition, it is unknown whether SGLT2 inhibitors work through glucose-dependent mechanisms or whether SGLT2 inhibitors could have an effect in patients without diabetes. Therefore, the effect of dapagliflozin, on top of standard care, was evaluated in HF patients with reduced ejection fraction (HFrEF) with and without diabetes.
The DAPA-HF trial enrolled 4744 HFrEF patients (symptomatic HF, EF ≤40%, NT-proBNP ≥600 pg/mL) and those with eGFR<30 mL/min/1.73m2, symptomatic hypotension, SBP <95 mmHg or type 1 diabetes were excluded. Primary endpoint was worsening HF event (unplanned HF hospitalization or an urgent HF visit requiring IV therapy) or CV death.
Main results
- Treatment with dapagliflozin resulted in a reduction of the primary endpoint of CV death and worsening HF event compared to placebo (HR: 0.74, 95%CI: 0.65-0.85, P=0.00001, NNT=21).
- All-cause death was reduced in the dapagliflozin group compared to the placebo group (HR: 0.83, 95%CI: 0.71-0.97, P=0.022).
- In the dapagliflozin group, percentage of patients with ≥5 point improvement in the Kansas City Cardiomyopathy Questionnaire (KCCQ) was increased and percentage of patients with ≥5 point deterioration was lowered compared to the placebo group.
- Individual endpoints (HF hospitalization/urgent HF visit, HF hospitalization, CV death, CV death/HF hospitalization, death from any cause) were all reduced in those who were on dapagliflozin compared to those who were on placebo.
- Dapagliflozin was well tolerated.
Conclusion
Dapagliflozin reduced the composite outcome of CV death and worsening HF event in HFrEF patients with and without diabetes in comparison to placebo. In addition, CV death was reduced and symptoms improved with dapagliflozin therapy compared to placebo. John McMurray concluded ‘this is an important breakthrough for patients with a terrible disease’.
Discussion
Although no data was presented on effect of dapagliflozin in diabetes patients vs. non-diabetes patients, McMurray said the reduction of the primary endpoint with dapagliflozin was identical in these two groups. This raised the question why dapagliflozin works in non-diabetes patients. McMurray proposed several mechanisms which include protection of the kidney, alteration of cardiac metabolism, the sodium hydrogen exchanger and there are probably many more.
In response to the question why this trial did enroll patients with T2DM instead of excluding them, McMurray responded that the investigators wanted to enroll typical HFrEF patients, and a large percentage has diabetes.
A consistent benefit of dapagliflozin was observed in patients using sacubitril/valsartan and those without this drug. McMurray said this was expected, as SGLT2 inhibitors work differently. This is great news, because there are now two new drugs.
- Our reporting is based on the information provided at the ESC congress -