Coronavirus infections and the cardiovascular system
This viewpoint article draws attention towards acute and possible long-term implications of coronavirus infections, such as COVID-19, on the cardiovascular system.
Coronaviruses and the cardiovascular system: acute and long-term implicationsLiterature - Xiong TY, Redwood S, Prendergast B, and Chen M - Eur Heart J. 2020. ehaa231, doi: 10.1093/eurheartj/ehaa231
CV complications of coronaviruses
Coronaviruses, including severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS) and COVID-19, have been associated with a significant burden of CV comorbidities and complications, such as myocardial injury, acute cardiac injury, shock, arrhythmia, acute myocarditis, acute heart failure and cardiac arrest [1-5]. A clinical cohort study involving 138 hospitalized COVID-19 patients showed that acute cardiac injury, shock, and arrhythmia were present in 7.2%, 8.7%, and 16.7 of patients, respectively [6]. The prevalence was higher among patients requiring intensive care.
Pathophysiology and possible implications on the CV system
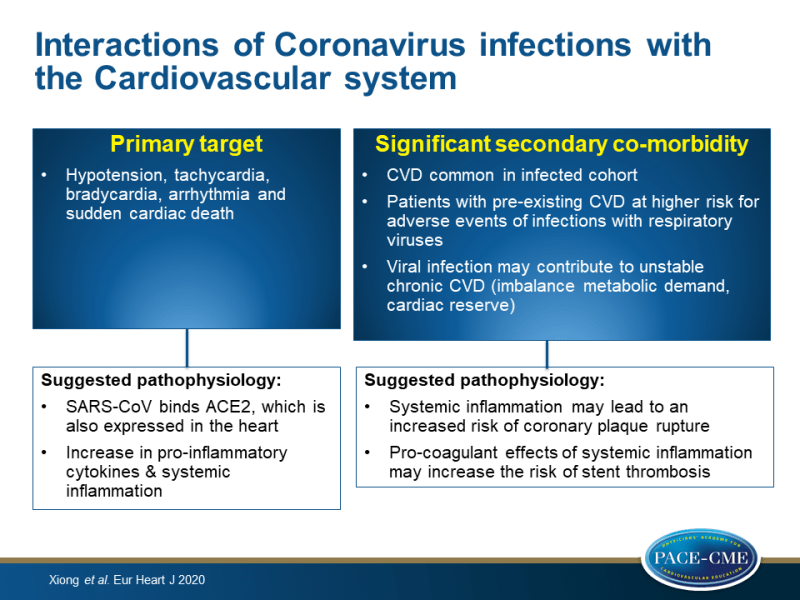
The beta-coronavirus underlying COVID-19 was named SARS-CoV-2 and strains from the same species as SARS. SARS-CoV binds to cells expressing viral receptors, particularly to angiotensin-converting enzyme 2 (ACE2) [7]. ACE2 is also expressed in the heart. Down-regulation of myocardial and pulmonary ACE2 pathways due to SARS-CoV infection can mediate myocardial inflammation, lung oedema and acute respiratory failure, as was shown in murine models and human autopsy samples [8]. As pro-inflammatory cytokines are upregulated in tissues of SARS patients, the systemic inflammatory response syndrome may lead to multi-organ failure, including the heart, in severe patients.
Viral infection may contribute to unstable chronic CVD due to an imbalance between infection-induced increase in metabolic demand and reduced cardiac reserve. Virally induced systemic inflammation may also lead to an increased risk of coronary plaque rupture in patients with coronary artery disease and heart failure. Furthermore, systemic inflammation can have pro-coagulant effects, which may increase the risk of stent thrombosis.
Long-term outcomes of respiratory viral infections
Clinical effects of pneumonia have been associated with increased risk of CVD up to 10-years follow-up [9]. Reports on long-term effects after recovery from a respiratory virus infection are scarce. Among 25 individuals who recovered from SARS, lipid metabolism remained disrupted up to 12 years after clinical recovery [10]. On the other hand, cardiac abnormalities that were observed in 8 patients with H7N9 influenza during hospitalization returned to normal within 1 year [11]. Scientific reports on viral phenotype, baseline clinical characteristics, disease severity and management impact are essential for the optimization of medical management and to improve short-term survival. However, follow-up studies following outbreaks of respiratory virus epidemics in patients that recovered from the index infection are also needed to gain insight in the long-term effects of possible extra-pulmonary manifestations.
Conclusion
Patients with pre-existing CVD may be at higher risk of adverse clinical outcomes of infections with respiratory viruses. Furthermore, these viral infections may have prolonged consequences for overall CV health. Interdisciplinary management of severe cases, especially in patients with pre-existing CVD, and long-term clinical follow-up is therefore important.
References
1. Yu C-M. Cardiovascular complications of severe acute respiratory syndrome. Postgrad Med J 2006;82:140–144.
2. Pan S, Zhang H, Li C, Wang C. [Cardiac arrest in severe acute respiratory syndrome: analysis of 15 cases]. Zhonghua Jie He He Hu Xi Za Zhi 2003;26: 602–605.
3. Li SS, Cheng C, Fu C, Chan Y, Lee M, Chan JW, Yiu S. Left ventricular performance in patients with severe acute respiratory syndrome: a 30-day echocardiographic follow-up study. Circulation 2003;108:1798–1803.
4. Alhogbani T. Acute myocarditis associated with novel Middle East respiratory syndrome coronavirus. Ann Saudi Med 2016;36:78–80.
5. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506.
6. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;doi:10.1001/jama.2020.1585.
7. Wit E D, Doremalen N. V, Falzarano D, Munster VJ. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol 2016;14:523–534.
8. Oudit GY, Kassiri Z, Jiang C, Liu PP, Poutanen SM, Penninger JM, Butany J. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest 2009;39:618–625.
9. Corrales-Medina VF, Alvarez KN, Weissfeld LA, Angus DC, Chirinos JA, Chang C-C, Newman A, Loehr L, Folsom AR, Elkind MS, Lyles MF, Kronmal RA, Yende S. Association between hospitalization for pneumonia and subsequent risk of cardiovascular disease. JAMA 2015;313:264.
10. Wu Q, Zhou L, Sun X, Yan Z, Hu C, Wu J, Xu L, Li X, Liu H, Yin P, Li K, Zhao J, Li Y, Wang X, Li Y, Zhang Q, Xu G, Chen H. Altered lipid metabolism in recovered SARS patients twelve years after infection. Sci Rep 2017;7:9110.
11. Wang J, Xu H, Yang X, Zhao D, Liu S, Sun X, Huang J, Guo Q. Cardiac complications associated with the influenza viruses A subtype H7N9 or pandemic H1N1 in critically ill patients under intensive care. Braz J Infect Dis 2017;21:12–18.
