Proposed new algorithm for sequencing drug treatments for HFrEF
John McMurray and Milton Packer proposed a new algorithm to achieve treatment with a beta-blocker, SGLT2i, ARNI and MRA within 4 weeks in patients with HFrEF.
How Should We Sequence the Treatments for Heart Failure and a Reduced Ejection Fraction? A Redefinition of Evidence-Based MedicineLiterature - McMurray JJV and Packer M, - Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.052926.
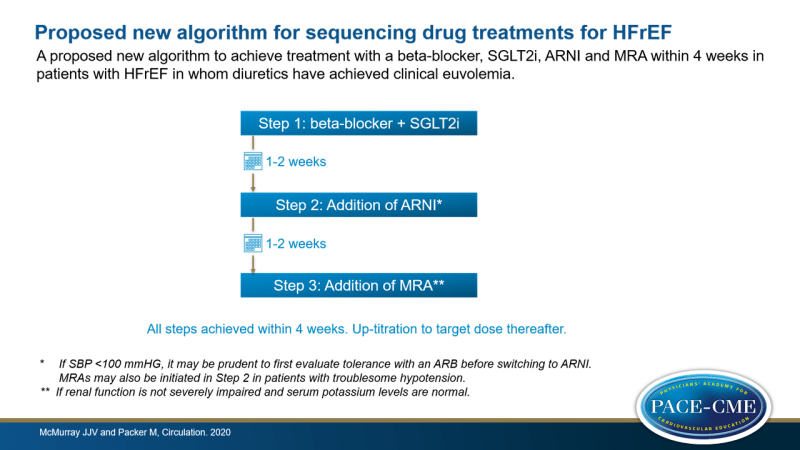
In a commentary article, John McMurray and Milton Packer proposed a new algorithm to achieve treatment with all four foundational treatments for HFrEF within 4 weeks. The proposed algorithm involves three steps and can be initiated in a patient in whom diuretics have achieved clinical euvolemia.
Proposed new algorithm:
- Step 1: Simultaneous initiation of a beta-blocker and an SGLT2i.
- Step 2: Addition of sacubitril/valsartan, within 1-2 weeks of Step 1. If SBP <100 mmHG, it may be prudent to first evaluate tolerance with an ARB before switching to ARNI.
- Step 3: Addition of an MRA, within 1-2 weeks of Step 2, if renal function is not severely impaired and serum potassium levels are normal. MRAs may also be initiated in Step 2 in patients with troublesome hypotension.
The algorithm can be individualized to specific circumstances and is most appropriate for outpatients. Caution is required in hospitalized patients with decompensated HF. This approach achieves treatment with beta-blocker, SGLT2i, ARNI and MRA within 4 weeks. Up-titration to target doses should be pursued after this period.
The new algorithm is based on five principles. First, the magnitude of the treatment benefit of each individual drug class is independent of the treatment benefits of other drug classes. Second, foundational drugs are effective in reducing morbidity and mortality at low starting doses [2-4]. Third, addition of a new drug class to the treatment yields greater benefit than up-titrating existing drug classes. Fourth, safety and tolerability can be improved by proper sequencing of drug classes [5]. Fifth, much of the benefit of foundational treatments can be seen within 30 days [2]. Therapy with all four drug classes should therefore be achieved within 4 weeks.
The conventional approach for treatment of HFrEF is to start with ACEi or ARB, to be followed by a beta-blocker, then an MRA, then an ARNI and then a SGLT2i. It is recommended to first reach the target dose of each drug class before adding the next recommended drug class. McMurray and Packer proposed the new algorithm because the conventional approach to achieving treatment with all four drug classes suffers from several limitations. First, The order to the prescribe the drugs is the precise sequence in which they were tested in clinical trials. The assumption that the most effective treatments were developed first, is not a strong rational for making therapeutic recommendations. Second, the conventional approach assumes that foundational treatments are effective only when titrated to target doses. However, benefits to reduce morbidity and mortality can already be reached at low doses. Target doses are often only modestly more effective in comparison with starting doses in reducing risk of CV death [1]. Third, the conventional approach assumes that clinical trials tested the efficacy and safety of each drug class in presence of all background therapies at target doses. The truth is that most patients in these trials were receiving sub-target doses of recommended treatment. Moreover, a substantial proportion of patients in most recently completed trials was not treated with an MRA or ARNI.
McMurray and Packer state that if physicians prioritize the achievement of target doses of each drug class before starting treatment with other drug classes, it takes several months to prescribe all recommended treatments. This delay is unacceptable since each of the drug classes has been shown to reduce morbidity and mortality within 30 days. The proposed new algorithm increases the likelihood that highly effective therapies are initiated within a month. McMurray and Packer expect that this will prevent HF death and HF hospitalizations and will enhance the tolerability of concurrently or subsequently administered treatments.
References
1. Packer M, Poole-Wilson PA, Armstrong PW, Cleland JG, Horowitz JD, Massie BM, Rydén L, Thygesen K, Uretsky BF. Comparative effects of low and high doses of the angiotensin-converting enzyme inhibitor, lisinopril, on morbidity and mortality in chronic heart failure. ATLAS Study Group. Circulation. 1999; 100: 2312-2318.
2. Lam PH, Packer M, Fonarow GC, Faselis C, Allman RM, Morgan CJ, Singh SN, Pitt B, Ahmed A. Early effects of starting doses of enalapril in patients with chronic heart failure in the SOLVD Treatment trial. Am J Med. 2020; 133: e25-e31.
3. Krum H, Roecker EB, Mohacsi P, Rouleau JL, Tendera M, Coats AJ, Katus HA, Fowler MB, Packer M; Carvedilol Prospective Randomized Cumulative Survival (COPERNICUS) Study Group. Effects of initiating carvedilol in patients with severe chronic heart failure: results from the COPERNICUS Study. JAMA. 2003; 289: 712-718.
4. Pitt B, White H, Nicolau J, Martinez F, Gheorghiade M, Aschermann M, van Veldhuisen DJ, Zannad F, Krum H, Mukherjee R, Vincent J; EPHESUS Investigators. Eplerenone reduces mortality 30 days after randomization following acute myocardial infarction in patients with left ventricular systolic dysfunction and heart failure. J Am Coll Cardiol. 2005; 46: 425-431.
5. Desai AS, Vardeny O, Claggett B, McMurray JJ, Packer M, Swedberg K, Rouleau JL, Zile MR, Lefkowitz M, Shi V, Solomon SD. Reduced risk of hyperkalemia during treatment of heart failure with mineralocorticoid receptor antagonists by use of sacubitril/valsartan compared with enalapril: a secondary analysis of the PARADIGM-HF trial. JAMA Cardiol. 2017; 2: 79-85.