ADA/EASD New Hyperglycemia Management Guidelines
25/04/2012
The American Diabetes Association and the European Association for the Study of Diabetes have updated guidelines on the management of hyperglycemia in nonpregnant adults with type 2 diabetes. Individualized treatment is the cornerstone of success
Management of Hyperglycemia in Type 2 Diabetes: A Patient-Centered Approach: Position Statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD).Literature - Inzucchi SE et al, Diabetes Care. 2012 Apr 19.
Inzucchi SE, Bergenstal RM, Buse JB, et al.
Diabetes Care. 2012 Apr 19. [Epub ahead of print]
The novel position statement on the management of hyperglycemia in type 2 diabetes was necessary because since the last similar treatment algorithm, which is more than 3 years old, a lot of new insights have been generated that required an update.
According to the ADA, to reduce the incidence of macrovascular disease, HbA1c should be lowered to less than 7% in most patients. However, data from type 2 diabetes cardiovascular trials have demonstrated that not all patients benefit from aggressive glucose maintenance, again pointing toward a more individualized approach to treatment. In considering patient desires and values, the following factors may be taken into account when choosing an HbA1c target: patient attitude and expected treatment efforts; risks potentially associated with hypoglycemia, other adverse events; disease duration; life expectancy; important comorbidities; established vascular complications; and resources and support systems.
For strong recommendations in favour (or against) certain diabetes medications, the evidence is not strong enough; choices and preferences will differ with different patients, their characteristics and attitudes. In contrast to previous statements, the present one is based on a patient-centered approach.
Several therapeutic options were discussed, including lifestyle interventions to change physical activity levels and food intake; oral agents and noninsulin injectables, as well as insulin. According to the guidelines, when it comes to prescribing oral agents and noninsulin injectables, agent- and patient-specific properties, such as dosing frequency, side effect profiles, cost and other benefits, are often used to guide drug selection.
In terms of insulin, an insulin treatment program should be designed specifically for an individual patient, to match the supply of insulin to his or her dietary/exercise habits and prevailing glucose trends, as revealed through self-monitoring. Anticipated glucose-lowering effects should be balanced with the convenience of the regimen, in the context of an individual’s specific therapy goals.
Metformin is the optimal first-line drug, unless there are established contraindications. After metformin, however, data are limited. The authors recommend combination therapy with the addition of one to two oral or injectable agents, with the goal of reducing side effects when possible. Insulin therapy, whether alone or in combination, will ultimately be required to maintain glucose control for many patients.
The second step can be a dipeptidyl peptidase-4 inhibitor, it can be a glucagon-like peptide-1 (GLP-1) receptor agonist, it can be a thiazolidinedione, it can be a sulfonylurea agent, or it could be basal insulin. Anything next can be tried depending on what suits the circumstance. Eventually, patients may need insulin alone, although in many cases, patients should still be on some sort of oral agent, and the combination of a GLP-1 receptor agonist and insulin is quite effective in many cases.
If a patient needs a more intensive insulin regimen, then it is recommended to add 1 or 2 - maybe even 3 - doses of mealtime insulin.
The position statement lists all commonly used medications with all their properties (positive and negative), and gives all the information to make good choices based on priorities (ie, avoiding hypoglycemia at all costs) and preferences. The authors hope this is valuable information to assist physicians treating patients with type 2 diabetes in ‘practicing the art of medicine.’
When making treatment decisions, additional considerations include age, weight, sex/racial/ethnic/genetic differences and comorbidities, such as coronary artery disease, heart failure, chronic kidney disease, liver dysfunction and hypoglycemia.
Overall, comparative evidence for antihyperglycemic treatment of type 2 diabetes is lacking, and there is a considerable need for high-quality, comparative-effectiveness research on costs and outcomes important to patients, including quality of life and the avoidance of life-limiting complications such as cardiovascular disease.
Diabetes Care. 2012 Apr 19. [Epub ahead of print]
Summary
- Glycemic targets and glucose-lowering therapies must be individualized.
- Diet, exercise, and education remain the foundation of any type 2 diabetes treatment program.
- Unless there are prevalent contraindications, metformin is the optimal first-line drug.
- After metformin, there are limited data to guide us. Combination therapy with an additional 1–2 oral or injectable agents is reasonable, aiming to minimize side effects where possible.
- Ultimately, many patients will require insulin therapy alone or in combination with other agents to maintain glucose control.
- All treatment decisions, where possible, should be made in conjunction with the patient, focusing on his/her preferences, needs, and values.
- Comprehensive cardiovascular risk reduction must be a major focus of therapy.
Background
The American Diabetes Association and the European Association for the Study of Diabetes have updated guidelines on the management of hyperglycemia in nonpregnant adults with type 2 diabetes. The update is based on new evidence of risks and benefits of glycemic control, evidence on safety and efficacy of new drug classes, the withdrawal and restriction of other drug classes and the increasing need for a more patient-centered approach to care. Individualized treatment is the cornerstone of success.The novel position statement on the management of hyperglycemia in type 2 diabetes was necessary because since the last similar treatment algorithm, which is more than 3 years old, a lot of new insights have been generated that required an update.
According to the ADA, to reduce the incidence of macrovascular disease, HbA1c should be lowered to less than 7% in most patients. However, data from type 2 diabetes cardiovascular trials have demonstrated that not all patients benefit from aggressive glucose maintenance, again pointing toward a more individualized approach to treatment. In considering patient desires and values, the following factors may be taken into account when choosing an HbA1c target: patient attitude and expected treatment efforts; risks potentially associated with hypoglycemia, other adverse events; disease duration; life expectancy; important comorbidities; established vascular complications; and resources and support systems.
For strong recommendations in favour (or against) certain diabetes medications, the evidence is not strong enough; choices and preferences will differ with different patients, their characteristics and attitudes. In contrast to previous statements, the present one is based on a patient-centered approach.
Several therapeutic options were discussed, including lifestyle interventions to change physical activity levels and food intake; oral agents and noninsulin injectables, as well as insulin. According to the guidelines, when it comes to prescribing oral agents and noninsulin injectables, agent- and patient-specific properties, such as dosing frequency, side effect profiles, cost and other benefits, are often used to guide drug selection.
In terms of insulin, an insulin treatment program should be designed specifically for an individual patient, to match the supply of insulin to his or her dietary/exercise habits and prevailing glucose trends, as revealed through self-monitoring. Anticipated glucose-lowering effects should be balanced with the convenience of the regimen, in the context of an individual’s specific therapy goals.
Metformin is the optimal first-line drug, unless there are established contraindications. After metformin, however, data are limited. The authors recommend combination therapy with the addition of one to two oral or injectable agents, with the goal of reducing side effects when possible. Insulin therapy, whether alone or in combination, will ultimately be required to maintain glucose control for many patients.
The second step can be a dipeptidyl peptidase-4 inhibitor, it can be a glucagon-like peptide-1 (GLP-1) receptor agonist, it can be a thiazolidinedione, it can be a sulfonylurea agent, or it could be basal insulin. Anything next can be tried depending on what suits the circumstance. Eventually, patients may need insulin alone, although in many cases, patients should still be on some sort of oral agent, and the combination of a GLP-1 receptor agonist and insulin is quite effective in many cases.
If a patient needs a more intensive insulin regimen, then it is recommended to add 1 or 2 - maybe even 3 - doses of mealtime insulin.
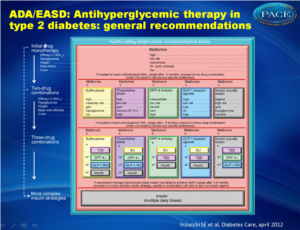 Antihyperglycemic therapy in type 2 diabetes:General recommendations, based on patient and drug characteristics.Click on image to enlarge |
The position statement lists all commonly used medications with all their properties (positive and negative), and gives all the information to make good choices based on priorities (ie, avoiding hypoglycemia at all costs) and preferences. The authors hope this is valuable information to assist physicians treating patients with type 2 diabetes in ‘practicing the art of medicine.’
When making treatment decisions, additional considerations include age, weight, sex/racial/ethnic/genetic differences and comorbidities, such as coronary artery disease, heart failure, chronic kidney disease, liver dysfunction and hypoglycemia.
Overall, comparative evidence for antihyperglycemic treatment of type 2 diabetes is lacking, and there is a considerable need for high-quality, comparative-effectiveness research on costs and outcomes important to patients, including quality of life and the avoidance of life-limiting complications such as cardiovascular disease.
