Arteriovenous anastomosis lowers blood pressure in uncontrolled hypertension
27/01/2015
Altering mechanical arterial properties contributing to chronic hypertension with an arteriovenous coupler yields BP reductions in patients with essential hypertension despite use of multiple antihypertensive drugs.
BackgroundLiterature - Lobo et al., The Lancet 2015
Central arteriovenous anastomosis for the treatment of patients with uncontrolled hypertension (the ROX CONTROL HTN study): a randomised controlled trial
Lobo MD, Sobotka PA, Stanton A, et al., for the ROX CONTROL HTN Investigators
The Lancet.Published online 22 January 2015.DOI: http://dx.doi.org/10.1016/S0140-6736(14)62053-5
In clinical settings, less than half of patients with hypertension achieve optimum blood pressure (BP) control despite treatment, and adherence is often not maintained in the long run [1-3]. Since even small increments in BP are associated with a higher cardiovascular (CV) risk, acceptable and effective treatment strategies are required.
Chronic hypertension may lead to arterial hypertrophy, which is associated with a loss of arterial compliance. Aortic stiffening is associated with increased BP variability, pulse pressure, and end organ damage [4], and is also associated with adverse CV events and mortality.
The novel arteriovenous ROX Coupler yields an immediate, substantial and sustained reduction of BP by adding a low-resistance, high-compliance venous segment to the central arterial tree, to benefit maximally from the natural mechanical effects [5-7]. Presented here are the results of a prospective, randomised trial in which creation of a central iliac arteriovenous anastomosis was evaluated with regard to its ability to safely lower BP in patients with uncontrolled hypertension. Patients in the control group did not undergo a procedure, but only continued current pharmaceutical treatment (as did the arteriovenous anastomosis group).
Main results
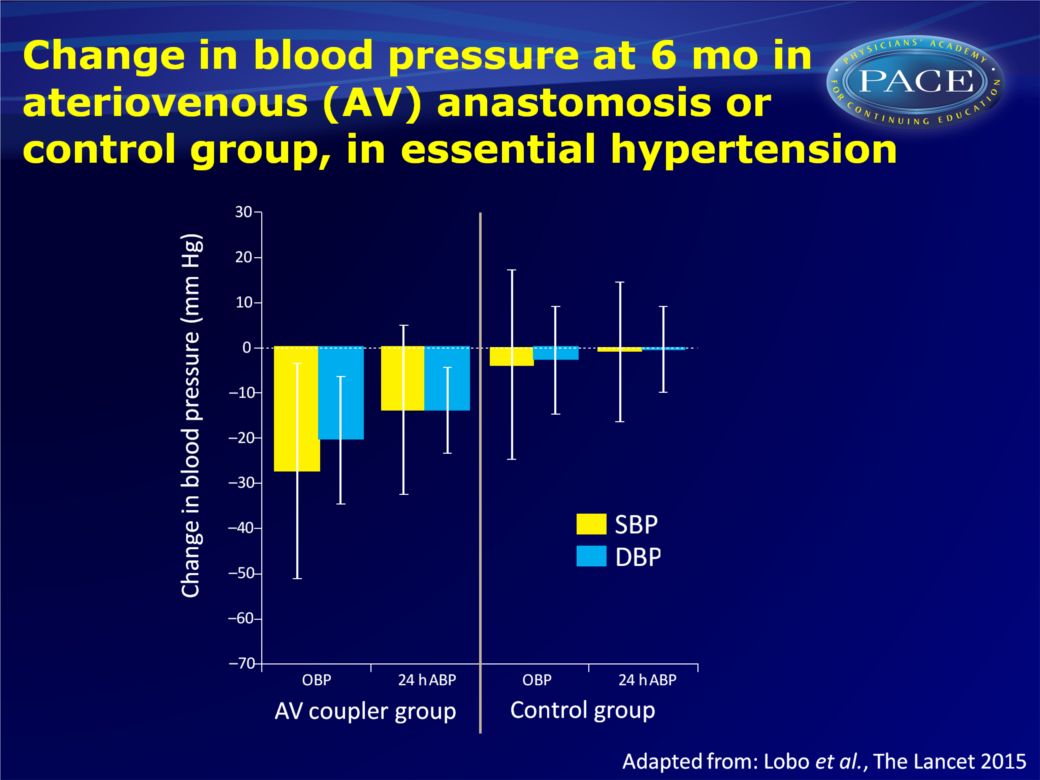
- Mean changes in office and 24h ambulatory BP after 6 months were significantly greater in the arteriovenous coupler group than in the control group (mean differences vs. control group: office BP: -23.2 mmHg SBP and -17.7 mmHg DBP, and ambulatory -13.0 mmHg SBP and -13.4 mmHg DBP).
- Day-time and night-time ambulatory BP were also significantly reduced in the arteriovenous coupler group as compared to the control group (daytime SBP: -13.9 vs. -1.5 mmHg and DBP: -14.7 vs. -1.1 mmHg, night-time SBP: -11.5 vs. 3.0 mmHg, and DBP: 10.0 vs. 2.5 mmHg).
- Among patients who had previously undergone renal denervation (RND), those in the arteriovenous coupler group had significantly decreased office and ambulatory SBP and DBP at 6 months, while control patients did not show significant changes at 6 months.
- 11 patients in the arteriovenous coupler group and 2 in the control group had the number of hypertension medications reduced, and 4 and 10 patients in the respective groups had to take more antihypertensive medications.
- An arteriovenous coupler was successfully placed in all but one of 43 randomised patients. In one patient placement was not attempted due to unsuitable anatomy. 25 procedure- or device-related adverse events were reported, two of which were serious. Late development of iliac vein stenosis proximal to the anastomosis occurred and was successfully treated in 12 patients.
Conclusion
In this study, an arteriovenous anastomotic coupler developed to alter the mechanical arterial properties contributing to chronic hypertension was associated with significant BP reductions in patients with uncontrolled essential hypertension despite use of multiple antihypertensive drugs. Both office and 24h ambulatory BP measures were improved at 6 months after the procedure.BP reductions were similar in those who had previously undergone and were unresponsive to RND, and those who had not. This suggests that inadequate response to RND may in part be the consequence of arterial stiffness. The current technique underlines the role of arterial compliance and vascular resistance abnormalities in patients with arterial hypertension, and warrants further study of safety and efficacy.
Find this article online at The Lancet
References
1 Irvin MR, Shimbo D, Mann DM, et al. Prevalence and correlates of low medication adherence in apparent treatment-resistant hypertension. J Clin Hypertens 2012; 14: 694–700.2 Van Wijk BL, Klungel OH, Heerdink ER, et al. Rate and determinants of 10-year persistence with antihypertensive drugs. J Hypertens 2005; 23: 2101–07.
3 Yiannakopoulou E, Papadopulos JS, Cokkinos DV, et al. Adherence to antihypertensive treatment: a critical factor for blood pressure control. Eur J Cardiovasc Prev Rehabil 2005; 12: 243–49.
4 Coutinho T, Turner ST, Kullo IJ. Aortic pulse wave velocity is associated with measures of subclinical target organ damage. JACC Cardiovasc Imaging 2011; 4: 754–61.
5 Faul J, Schoors D, Brouwers S, et al. Creation of an iliac arteriovenous shunt lowers blood pressure in chronic obstructive pulmonary disease patients with hypertension. J Vasc Surg 2014; 59: 1078–83
6 Cooper CB, Celli B. Venous admixture in COPD: pathophysiology and therapeutic approaches. COPD 2008; 5: 376–81.
7 Burchell AE, Lobo MD, Sulke N, et al. Arteriovenous anastomosis: is this the way to control hypertension? Hypertension 2014; 64: 6–12.
