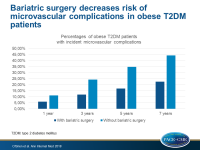
Bariatric surgery decreases risk of microvascular complications in obese diabetic patients
Obese patients with T2DM, who underwent bariatric surgery, had a two-fold risk reduction of microvascular complications compared with matched controls.
Microvascular Outcomes in Patients With Diabetes After Bariatric Surgery Versus Usual CareLiterature - O’Brien R, Johnson E, Haneuse S et al. - Ann Intern Med 2018; published online ahead of print
Introduction and methods
Bariatric surgery leads often to remission of type 2 diabetes mellitus (T2DM), but there are conflicting data regarding its effect on microvascular complications [1-3]. This retrospective, observational, matched cohort study assessed whether bariatric surgery was associated with lower incidence of microvascular disease than usual care for patients with severe obesity and T2DM.
For this purpose, patients with T2DM, aged 19-79 years, with a body mass index (BMI) ≥35 kg/m2, who had primary bariatric surgery between 2005 and 2011, were identified in four health care system databases. T2DM was defined as hemoglobin A1c level ≥6.5% or fasting plasma glucose level ≥6.99 mmol/L (126 mg/dL), or a current prescription for any diabetes medication.
Patients with less than one full year of continuous enrollment, those with a history of gastrointestinal surgery for cancer, pregnancy in the year before surgery, gestational diabetes as the sole diabetes diagnosis, metformin as the sole indicator of possible T2DM, preexisting neuropathy, retinopathy, or nephropathy, as well as those with missing data or those who could not be matched with a control were excluded from this analysis, leaving a sample of 4,024 patients.
Patients who underwent bariatric surgery were matched 1:3 with controls, consisting of T2DM patients with a BMI ≥35 kg/m2, who did not have bariatric surgery. The primary outcome measure was time to incident microvascular disease (composite of first occurrence of retinopathy, neuropathy, or nephropathy). Nephropathy was defined by at least two measures of estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2 separated by at least 90 days, without any intervening values of ≥60 mL/min/1.73 m2. eGFR was approximated using serum creatinine values and the CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) equation [4]. The mean follow-up was 4.3 years.
Main results
- The rates of incident microvascular disease after bariatric surgery at 1, 3, 5, and 7 years were 6.0%, 11.8%, 16.9%, and 22.5%, respectively, and 11.2%, 24.3%, 34.7%, and 44.2% in the control group.
- At 5 years, the risk for incident microvascular disease was significantly lower in surgical patients compared with controls (HR for all: 0.41; CI: 0.34-0.48; HR for diabetic neuropathy: 0.37; CI: 0.30-0.47; HR for nephropathy: 0.41; CI: 0.29-0.58; HR for retinopathy: HR: 0.55; CI: 0.42-0.7]).
Conclusion
Adult, obese T2DM patients, who underwent bariatric surgery, had a reduced risk of microvascular complications compared with matched obese T2DM without surgery.
Editorial comment
In his editorial article, le Roux [5] discusses the limitations of the study published by O’Bien et al., which include the possible misclassifications of diagnoses and selection bias when using an electronic database, the need to determine the additive effectiveness of bariatric surgery in combination with medical therapy, as well as the use of a creatinine-based biomarker as a measurement for renal function, which, however, improves after bariatric surgery, independently from the renal function per se. The author concludes: ‘Bariatric surgery is safe and is, at present, our most evidence-based treatment to put hyperglycemia from T2DM into remission. We are on the verge of having the data to tell our patients with T2DM in the clinic that we can offer them a treatment that significantly reduces the feared complications of this dreadful disease. Surgery should not be a last resort but instead should be used earlier, because prevention is definitely better than cure.’
References
1. Schauer PR, Bhatt DL, Kirwan JP, et al; STAMPEDE Investigators. Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. N Engl J Med. 2017;376:641-51.
2. Coleman KJ, Haneuse S, Johnson E, et al. Long-term microvascular disease outcomes in patients with type 2 diabetes after bariatric surgery: evidence for the legacy effect of surgery. Diabetes Care. 2016;39:1400-7.
3. Carlsson LMS, Sjoholm K, Karlsson C, et al. Long-term incidence of microvascular disease after bariatric surgery or usual care in patients with obesity, stratified by baseline glycaemic status: a post-hoc analysis of participants from the Swedish Obese Subjects study. Lancet Diabetes Endocrinol. 2017;5:271-9.
4. Matsushita K, Mahmoodi BK, Woodward M, et al; Chronic Kidney Disease Prognosis Consortium. Comparison of risk prediction using the CKD-EPI equation and the MDRD study equation for estimated glomerular filtration rate. JAMA. 2012;307:1941-51.
5. le Roux CW. Prevention Is Better Than Cure: The Next Frontier for Bariatric Surgery? Ann Intern Med 2018; published online ahead of print.