 Current Situation
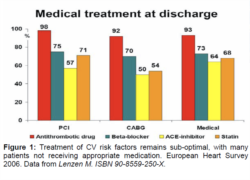
The most recent European Heart Survey has reported that patients are still not treated optimally, with only 50-60% of patients receiving ACEI and statins6 (Figure 1). At the same time, the German DUTY register of 51,000 diabetics revealed that more than 54% had an HbA1c >7%, blood pressure exceeded 140/90 mmHg in 65% and LDL-C was >100mg/dl in 84%7, revealing that these patients are not achieving guideline goals and this is a matter of some concern. Yet even when patients are treated well, diabetic patients continue to suffer high event rates, evidenced in the BARI-2D trial, in which patients maintained an acceptable HbA1c level (7.5%), LDL 80mg, BP 125/70 mmHg, GFR 70 ml/min and mean BMI of 32 kg/m2. Despite this, the event rates remained high over the 5 year trial, reporting MACE at 24%, CHF 22% and mortality at 12%8. ACCORD and ADVANCE failed to demonstrate that tight glucose control alone improves macrovascular risk, whilst the combination of metformin and sulphonylureas (SUs) might have actually increased CV risk9. As a result of the high CV risk in such patients and the negative outcome results seen with the older conventional anti-diabetic agents, it is important to give more attention to positive outcome studies, such as seen with pioglitazone. |