Child-to-adult BMI trajectories affect CV risk factors in mid-adulthood
Obesity in childhood that persists or worsens during adulthood is associated with higher risks of developing hypertension, T2DM, and dyslipidemia.
Distinct child-to-adult body mass index trajectories are associated with different levels of adult cardiometabolic riskLiterature - Buscot M-J, Thomson RJ, Juonala M, et al. - Eur Heart J 2018; published online ahead of print
Introduction and methods
Overweight and obese children have a higher CV risk, and there are data suggesting that those who achieve a normal weight between childhood and adulthood have normalization of adult CV risk [1]. Relevant studies have used body mass index (BMI) at single or limited number of time points as a measure [2], therefore, it is not known, how fluctuations of BMI through lifetime impact CV risk.
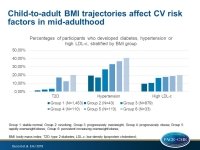
In this analysis of the 31-year prospective Cardiovascular Risk in Young Finns Study (YFS) [3,4], subgroups of participants were identified who share similar trajectories in BMI from childhood through mid-adulthood: the ‘stable normal’ (Group 1: N=1453; 55.2%), the ‘resolving’ (Group 2: N=43; 1.6%), the ‘progressively overweight’ (Group 3: N=879; 33.4%), the ‘progressively obese’ (Group 4: N=110; 4.2%), the ‘rapidly overweight/obese’ (Group 5: N=113; 4.3%), and the ‘persistently increasing overweight/obese’ (Group 6: N=33; 1.2%).
The independent association of these BMI trajectories with adult CV disease outcomes of type 2 diabetes mellitus (T2DM), hypertension, high-risk lipid levels and high-risk carotid intima-thickness (dMT) was evaluated. For this purpose, a YFS subset of 2631 YFS participants (aged 6–18 years in 1980 and 34-49 years at the latest follow-up in 2011) with ≥3 height and weight measurements between 1980 and 2011 was selected.
Main results
- Compared with participants classified in group 1, all BMI classes with worsening or persisting obesity (i.e. group 3–6) had significantly higher risk for all considered adult CVD outcomes.
- For group 2, RRs for hypertension, LDL-c and HDL-c were similar to group 1 and RR for T2DM was increased (RR: 2.13, 95%CI:0.14-8.23).
- Compared with group 1, group 2 had an approximately 3.5 higher risk to develop abnormal cIMT (RR: 3.37; 95%CI: 1.8-6.39, P<0.01).
- The percentages of participants who developed hypertension were 19.3% in group 1, 17.1% in group 2, 26.9% in group 3, 33.1% in group 4, 36.5% in group 5, and 40.6% in group 6.
- Compared with group 2, groups 4, 5, and 6 had a higher risk to develop hypertension (RR4: 1.7; 95%CI: 1.2-2.4; RR5: 1.9; 95%CI: 1.4-2.6; RR6: 2.5; 95%CI: 1.6-4.1).
- The percentages of participants who developed high LDL-c levels were 9.4% in group 1, 10.5% in group 2, 16.5% in group 3, 17.9% in group 4, 18.7% in group 5, and 19.8% in group 6.
- Compared with group 2, groups 4-6 had a higher risk to develop high LDL-c levels (RRs ranging from 1.6 to 1.8).
- The percentages of participants who developed T2DM were 1.4% in group 1, 2.6% in group 2, 3.5% in group 3, 17.1% in group 4, 12.6% in group 5, and 20.1% in group 6.
- Compared with group 2, the risk of developing T2DM was 5 to 7 times higher in group 4 (RR: 4.8; 95%CI: 1.1-20.8) and in group 6 (RR: 7.3; 95%CI: 1.3-34.2).
Conclusion
Obesity in childhood that persists or worsens during adulthood is associated with higher risks of developing hypertension, T2DM, and dyslipidemia, but results for individual cardiometabolic risk factors are not all consistent in direction. Achieving normal weight between childhood and adulthood is associated with lower risks, although the effect of youth obesity on the risk of adult pre-atherosclerosis may not be reversible.
Editorial comment
In their editorial article, Charakida and Deanfield [5] note that BMI is not the ideal measure of adiposity, since it does not account for body fat distribution. They also note that less than 2% of participants were in group 2, and therefore relevant results should be interpreted with caution. The authors conclude: ‘Weight loss is important and should be encouraged at any stage in life to reduce CVD risk. As early life factors can be crucial in setting up lifelong BMI trajectories, screening programmes and initiatives to tackle obesity should start in the young. Children, however, are intellectually and psychologically immature compared with adults and more susceptible to peer pressures. Success in targeting obesity is, therefore, unlikely to be achieved simply by educating children. Improved public awareness, together with initiatives to educate both families and primary care physicians about the link between BMI trajectories and long-term CVD risk, are a priority.’
References
1. Mattsson N, Ronnemaa T, Juonala M, et al. Childhood predictors of the metabolic syndrome in adulthood. The Cardiovascular Risk in Young Finns Study. Ann Med 2008;40:542–552.
2. Nadeau KJ, Maahs DM, Daniels SR, et al. Childhood obesity and cardiovascular disease: links and prevention strategies. Nat Rev Cardiol 2011;8:513–525.
3. Juonala M, Viikari JS, Raitakari OT. Main findings from the prospective Cardiovascular Risk in Young Finns Study. Curr Opin Lipidol 2013;24:57–64.
4. Raitakari OT, Juonala M, Ronnemaa T, et al. Cohort profile: the cardiovascular risk in Young Finns Study. Int J Epidemiol 2008;37:1220–1226.
5. Charakida M and Deanfield JE. BMI trajectories from childhood: the slippery slope to adult obesity and cardiovascular disease. Eur Heart J 2018; published online ahead of print.