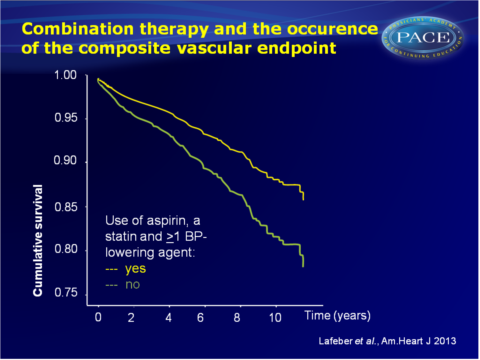
Combination therapy consisting of statin, aspirin and >1 BP-lowering agent reduces CV-risk
Using three components is more effective at reducing CV events and mortality than taking one or two components of combination therapy, in patients with established CAD.
The combined use of aspirin, a statin, and blood pressure–lowering agents (polypill components) and the risk of vascular morbidity and mortality in patients with coronary artery diseaseLiterature - Lafeber M, Spiering W, Van der Graaf Y et al. - Am. Heart J. 2013.166 (2): 282-289.e1
Lafeber M, Spiering W, Van der Graaf Y et al.
Am. Heart J. 2013.166 (2): 282-289.e1
Background
European guidelines for risk factor treatment in patients with established coronary artery disease (CAD) recommend the combined use of antiplatelet therapy, lipid-lowering agents (when LDL-c>2.5 mmol/L), a beta-blocker and additional blood pressure (BP)-lowering drugs if systolic BP>140mmHg [1]. In clinical practice, a large gap exists between indicated therapy and prescribed medication, and ineffective therapies are specifically common in middle- and low-income countries [2,3]. Suboptimal adherence to medication by patients further complicates matters [4]. Adherence to medication is inversely related to the number of pills and the number of doses per day [5,6].A fixed-dose combination pill containing aspirin, a statin and >1 BP-lowering agents could help to optimize the prevention of CV disease. Recent studies investigating such cardiovascular polypills in patients with a low and intermediate risk of CVD showed that they are safe, effective in reducing risk factors and at reducing the risk [7-9].
While waiting for the results of ongoing randomised trials testing the effectiveness, adherence and clinical outcomes of combination pills that should lower LDL-c and BP, this cohort study aimed to evaluate the combined use of aspirin, a statin and >1 BP-lowering agent in patients with CAD in clinical practice. Data of 2706 patients enrolled in the prospective Second Manifestations of ARTerial disease (SMART) cohort [10] were used, with a median follow-up time of 5.0 years.
Main results
- Combination therapy was associated with a lower risk of MI (HR: 0.68, 95%CI: 0.49-0.96), ischemic cerebrovascular accident (iCVA) (HR:0.37, 95%CI: 0.16-0.84), composite vascular endpoint (HR: 0.66, 95%CI: 0.49-0.88), vascular mortality (HR: 0.53, 95%CI:0.33-0.85) and all-cause mortality (HR: 0.69, 95%CI: 0.49-0.96), as compared to lack of combination therapy.
- Different variations of partial combination therapy were seen, often despite there being an indication for combination therapy based on the medical history.
- As compared to taking combination therapy of all 3 components, using only 2 components gave a higher risk of MI (HR: 1.42, 95%CI:1.00-2.03). Taking only 1 component also yielded a higher risk of MI (HR: 1.95, 95%CI: 1.09-3.50). Similar outcomes were seen for the composite vascular end point, vascular mortality and all-cause mortality.
Download Lafeber Polypill PACE.pptx or click to enlarge
Conclusion
In a population of patients with established vascular disease, the combined use of aspirin, a statin and >1 BP-lowering agent is associated with a lower risk of vascular events and all-cause mortality. Taking only one or two components of combination therapy did not give the same cardiovascular protection. These observations strengthens the hypothesis that combination therapy reduces the risk of CV events. Results of ongoing trials assessing the effectiveness of these polypills to improve CV clinical outcome should however be awaited before implementing this strategy in daily practice.References
1. Graham I, Atar D, Borch-Johnsen K, et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Eur Heart J 2007;28:2375-414.
2. Kotseva K, Wood D, De Backer G, et al. Cardiovascular prevention guidelines in daily practice: a comparison of Euroaspire I, II, and III surveys in eight European countries. Lancet 2009;373:929-40.
3. Yusuf S, Islam S, Chow CK, et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middleincome, and low-income countries (the pure study): a prospective
epidemiological survey. Lancet 2011;378(9798):1231-43.
4. Newby LK, LaPointe NM, Chen AY, et al. Long-term adherence to evidence-based secondary prevention therapies in coronary artery disease. Circulation 2006;113:203-12.
5. Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther 2001;23:1296-310.
6. Coleman CI, Roberts MS, Sobieraj DM, et al. Effect of dosing frequency on chronic cardiovascular disease medication adherence. Curr Med Res Opin 2012;28(5):669-80.
7. Yusuf S, Pais P, Afzal R, et al. Effects of a polypill (polycap) on risk factors in middle-aged individuals without cardiovascular disease (tips): a phase II, double-blind, randomised trial. Lancet 2009;373:1341-51.
8. Malekzadeh F, Marshall T, Pourshams A, et al. A pilot double-blind randomised placebo-controlled trial of the effects of fixed-dose combination therapy (‘polypill’) on cardiovascular risk factors. Int J Clin Pract 2010;64:1220-7.
9. Rodgers A, Patel A, Berwanger O, et al. An international randomized placebo-controlled trial of a four-component combination pill (“polypill”) in people with raised cardiovascular risk. PLoS One 2011;6:e19857.
10. Simons PC, Algra A, van de Laak MF, et al. Second manifestations of arterial disease (smart) study: rationale and design. Eur J Epidemiol 1999;15:773-81.
