Coronary atheroma volume associated with MACE, despite target LDL-c levels
Atherosclerotic disease burden remains an informative prognostic factor, even when LDL -c<70mg/dL is obtained with high-intensity statin treatment.
Coronary atheroma volume and cardiovascular events during maximally intensive statin therapyLiterature - Puri R, Nissen SE, Shao M, et al. - Eur Heart J. 2013 Jul 25
Puri R, Nissen SE, Shao M, et al
Eur Heart J. 2013 Jul 25
Background
The burden of atherosclerosis is related to the majority of ischemic cardiovascular events. Intravascular ultrasound (IVUS) is an imaging technique that yields high-resolution, precise volumetric quantification of epicardial coronary atherosclerosis. IVUS can help evaluate the potential anti-atherosclerotic efficacy of interventions on plaque development, by measuring the change in atheroma volume over time [1].High-dose statin therapy halts the progression [2], and regresses coronary atherosclerosis [3,4] and lowers clinical event rates [5,6], but in many patients a residual risk remains. The baseline coronary atheroma volume measured with IVUS associates with adverse CV events [7], but the prognostic significance of atheroma burden in patients treated with intensive statin therapy is unclear.
The Study of Coronary Atheroma by Intravascular Ultrasound: Effect of Rosuvastatin vs. Atorvastatin (SATURN) assessed progression of coronary atherosclerosis in patients treated with the highest doses of atorvastatin and rosuvastatin [4]. This analysis determined the relationship between IVUS-derived baseline coronary atheroma volume and subsequent major adverse CV events (MACE) in patients achieving very low LDL-c levels with high-intensity statin therapy. Patients had angiographically demonstrable coronary disease and LDL-c<116 mg/dL following a 2-week treatment period with atorvastatin 40 mg or rosuvastatin 20 mg daily, and were re-randomised and treated for 24 months with atorvastatin 80 mg or rosuvastatin 40 mg daily. IVUS imaging was performed at baseline and after 104 weeks of treatment.
Main results
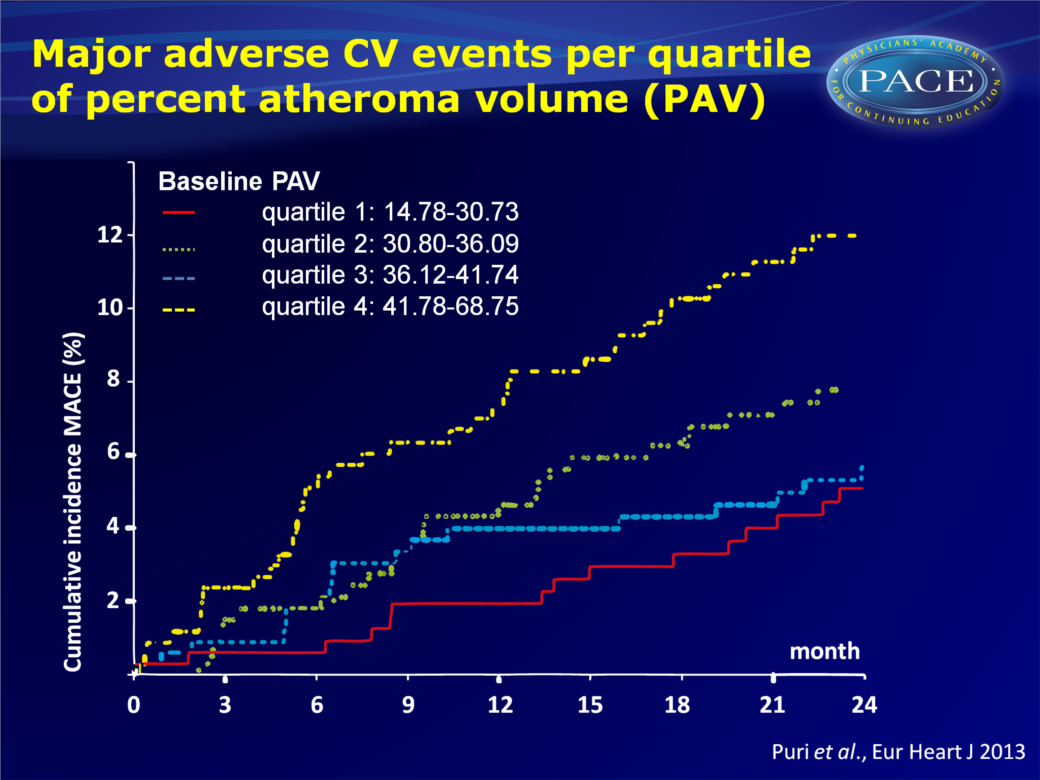
- The proportion of total vessel wall volume occupied by the atherosclerotic plaque is termed percent atheroma volume (PAV). Patients with baseline PAV above median had comparable LDL-c levels to those with PAV below the median (119.0+29 vs. 121.0+27 mg/dL, P=0.09), as well as at follow-up (65.3+23 vs. 65.8+22 mg/dL, P=0.47).
- Patients with a higher baseline PAV started with lower baseline HDL-c (43.7+10.8 vs. 46.3+11.6 mg/dL, P.001), but showed a greater increase during follow-up (13.0+18.9 vs. 9.7+17.6%, P=0.002) than those with PAV below the median. Similarly, they had lower apoA-1 levels at baseline (124.7+23.4 vs. 129.6+24.9 mg/dL, P=0.005) and showed a larger increase (14.6+18.9 vs. 9.7+17.6%, P=0.002) than patients with lower PAV.
- Patients with PAV above median at baseline showed a larger reduction in PAV (-1.50+0.17 vs. -0.87+0.17%, P=0.03) than patients with lower PAV.
- Baseline PAV correlated significantly with occurrence of MACE (HR: 1.28, 95%CI: 1.05-1.57, P=0.01), whereas baseline and on-treatment LDL-c levels did not associate with MACE.
- Patients in the highest quartile of baseline PAV (>41.8%) had a 2-year cumulative incidence of MACE of 12%, as compared to 5.7, 7.9 and 5.1% for the respective lower quartiles.
Click to enlarge or to download slide
Conclusion
This study shows that, although LDL-c<70mg/dL was obtained with high-intensity statin treatment, baseline coronary atheroma volume remained associated with subsequent MACE. Higher PAV was associated with more cumulative MACE. Thus, atherosclerotic disease burden remains an informative prognostic factor. These findings confirm the need for anti-atherosclerotic therapeutic strategies beyond LDL-c lowering.References
1. Tardif JC, Lesage F, Harel F,et al. Imaging biomarkers in atherosclerosis trials. Circ Cardiovasc Imaging 2011;4:319–333.
2. Nissen SE, Tuzcu EM, Schoenhagen P, et al. Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: a randomized controlled trial. JAMA 2004;291:1071–1080.
3. Nissen SE, Nicholls SJ, Sipahi I, et al. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA 2006;295:1556–1565.
4. Nicholls SJ, Ballantyne CM, Barter PJ, et al. Effect of two intensive statin regimens on progression of coronary disease. N Engl J Med 2011;365:2078–2087.
5. Cannon CP, Braunwald E, McCabe CH, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med 2004;350:1495–1504.
6. LaRosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med 2005;352:1425–1435.
7. Nicholls SJ, Hsu A, Wolski K,et al. Intravascular ultrasound-derived measures of coronary atherosclerotic
plaque burden and clinical outcome. J Am Coll Cardiol 2010;55:2399–2407.
