Cost-effectiveness of options for the diagnosis of high blood pressure in primary care
Ambulatory monitoring was the most cost-effective strategy for the diagnosis of hypertension for men and women of all ages. Lancet. 2011 Oct
Cost-effectiveness of options for the diagnosis of high blood pressure in primary care: a modelling study.News - Oct. 5, 2011
Lancet. 2011 Oct 1;378(9798):1219-30
The diagnosis of hypertension has traditionally been based on blood-pressure measurements in the clinic, but home and ambulatory measurements better correlate with cardiovascular outcome, and ambulatory monitoring is more accurate than both clinic and home monitoring in diagnosing hypertension. We aimed to compare the cost-effectiveness of different diagnostic strategies for hypertension.
Methods:
We did a Markov model-based probabilistic cost-effectiveness analysis. We used a hypothetical primary-care population aged 40 years or older with a screening blood-pressure measurement greater than 140/90 mm Hg and risk-factor prevalence equivalent to the general population. We compared three diagnostic strategies-further blood pressure measurement in the clinic, at home, and with an ambulatory monitor-in terms of lifetime costs, quality-adjusted life years, and cost-effectiveness.
Findings:
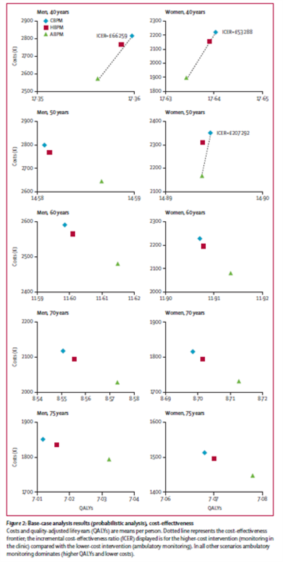
Ambulatory monitoring was the most cost-effective strategy for the diagnosis of hypertension for men and women of all ages. It was cost-saving for all groups (from -£56 [95% CI -105 to -10] in men aged 75 years to -£323 [-389 to -222] in women aged 40 years) and resulted in more quality-adjusted life years for men and women older than 50 years (from 0•006 [0•000 to 0•015] for women aged 60 years to 0•022 [0•012 to 0•035] for men aged 70 years). This finding was robust when assessed with a wide range of deterministic sensitivity analyses around the base case, but was sensitive if home monitoring was judged to have equal test performance to ambulatory monitoring or if treatment was judged effective irrespective of whether an individual was hypertensive.
Interpretation: Ambulatory monitoring as a diagnostic strategy for hypertension after an initial raised reading in the clinic would reduce misdiagnosis and save costs. Additional costs from ambulatory monitoring are counterbalanced by cost savings from better targeted treatment. Ambulatory monitoring is recommended for most patients before the start of antihypertensive drugs.
Background
High blood pressure is a key risk factor for the development of cardiovascular disease,1 and a major cause of morbidity and mortality worldwide.2 Hypertension is the most common reason for a primary-care consultation for a chronic disorder, and at least 25% of adults are hypertensive.3,4 The diagnosis of hypertension has traditionally been based on several blood-pressure measurements made in the clinic, which are typically undertaken after a raised initial reading.5–9 Ambulatory blood-pressure monitoring better correlates with cardiovascular outcome10–12 than does clinic blood pressure, and it is used where there is uncertainty in diagnosis, resistance to treatment, irregular or diurnal variation, or concerns about variability and the so-called white-coat effect.13–15 Therefore, ambulatory monitoring is arguably the de facto reference standard for the diagnosis of hypertension. Moreover, recent analyses suggest that ambulatory monitoring is more accurate than both monitoring in the clinic and the home in defining the presence of hypertension and could therefore form part of the diagnostic pathway.16 Home blood-pressure monitoring, which provides many readings over several days, also better correlates with end-organ damage than measurement in the clinic.17,18 Monitoring in the home seems a better prognostic indicator with respect to stroke and cardiovascular mortality than monitoring in the clinic and can detect the white-coat effect and masked hypertension.19–21 Although monitoring at home has a smaller evidence base, it might provide an appropriate alternative to ambulatory monitoring in terms of diagnosis, particularly in primary care where ambulatory monitoring is not always immediately available or when patients find it inconvenient or uncomfortable. The aim of this study was to develop a model to assess the cost-effectiveness of three diagnostic strategies for hypertension after a raised initial clinic blood-pressure reading: further blood-pressure measurement in the clinic, at home, or with an ambulatory monitor.
Main results
Ambulatory monitoring was the most cost-effective strategy form men and women of all ages. It was cost-saving in all groups and resulted in improved health outcomes for male and female age groups older than 50 years. In younger age groups, ambulatory monitoring had greater cost savings but was associated with a small reduction in QALYs; however, it was still the most cost-effective option because the incremental cost-effectiveness ratios associated with a clinic diagnosis compared with ambulatory monitoring were greater than £50 000 per QALY (figure). For home monitoring, both quality of life and costs were similar compared with clinic diagnosis at all ages in both men and women. The savings with ambulatory monitoring compared with monitoring in the clinic and the home were primarily because of the costs of hypertensive treatment that were avoided because of the higher specificity of ambulatory monitoring.
A wide range of deterministic sensitivity analyses varying the base-case assumptions and inputs also showed ambulatory monitoring remained the most cost-effective strategy in most circumstances, including those analyses in which the cost of ambulatory monitoring was varied. The superiority of ambulatory monitoring was also somewhat sensitive to the assumption that subsequent blood-pressure checks for people diagnosed as being without hypertension are undertaken every 5 years. Ambulatory monitoring was no longer the dominant strategy when such checks, and hence potentially repeated ambulatory monitoring, were done annually. Home monitoring became more cost-effective in the younger subgroups, although ambulatory monitoring remained the most cost-effective in older subgroups because of the QALY gain.
Conclusion
Ambulatory monitoring is the most cost-effective diagnostic strategy for confirming the diagnosis of hypertension across a range of age subgroups in both men and women. In most subgroups, ambulatory monitoring both improved health (increased QALYs) and reduced costs. Ambulatory monitoring for most people before the start of antihypertensive treatment should be seriously considered.
References
1. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903–13.
2. Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ, and the Comparative Risk Assessment Collaborating Group. Selected major risk factors and global and regional burden of disease. Lancet 2002; 360: 1347–60.3. Department of Health. Health survey for England 2003—trends. London: Department of Health, 2004.http://www.dh.gov.uk/en/PublicationsAndStatistics/PublishedSurvey/HealthSurveyForEngland/HealthSurveyResults/DH_4098913 (accessed June 11, 2011).
4. Information Centre for Health and Social Care. The quality and outcomes framework 2006/7. http://www.ic.nhs.uk/statistics-anddata-collections/audits-and-performance/the-quality-and-outcomesframework/the-quality-and-outcomes-framework-2006-07 (accessed Aug 8, 2011).
5. NICE. Hypertension: management of hypertension in adults in primary care—clinical guidelines CG34. London: National Institute for Clinical Excellence, 2006. http://www.nice.org.uk/guidance/index.jsp?action=byID&o=10986 (accessed June 11, 2011).
6. Williams B, Poulter NR, Brown MJ, et al. Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004-BHS IV. J Hum Hypertens 2004; 18: 139–85.
7. US Department of Health and Human Services. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure—complete report http://www.nhlbi.nih.gov/guidelines/hypertension/jnc7full.htm (accessed June 11, 2011).
8. National Collaborating Centre for Chronic Conditions. Hypertension: management in adults in primary care: pharmacological update. London: Royal College of Physicians, 2006.
9. Mancia G, De Backer G, Dominiczak A, et al, and the Management of Arterial Hypertension of the European Society of Hypertension, and the European Society of Cardiology. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25: 1105–87.
10. Ohkubo T, Hozawa A, Nagai K, et al. Prediction of stroke by ambulatory blood pressure monitoring versus screening blood pressure measurements in a general population: the Ohasama study. J Hypertens 2000; 18: 847–54.
11. Staessen JA, Thijs L, Fagard R, et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure
in older patients with systolic hypertension. JAMA 1999; 282: 539–46.
12. Imai Y, Ohkubo T, Sakuma M, et al. Predictive power of screening blood pressure, ambulatory blood pressure and blood pressure measured at home for overall and cardiovascular mortality: a prospective observation in a cohort from Ohasama, northern Japan. Blood Press Monit 1996; 1: 251–4.
13. Whitworth JA. 2003 World Health Organization (WHO)/ International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens 2003; 21: 1983–92.
14. Verdecchia P. Reference values for ambulatory blood pressure and self-measured blood pressure based on prospective outcome data. Blood Press Monit 2001; 6: 323–27.
15. Redon J, Campos C, Narciso ML, Rodicio JL, Pascual JM, Ruilope LM. Prognostic value of ambulatory blood pressure monitoring in refractory hypertension: a prospective study. Hypertension 1998; 31: 712–18.
16. Hodgkinson J, Mant J, Martin U, et al. Relative eff ectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: systematic review. BMJ 2011; 342: d3621.
17. Mulè G, Caimi G, Cottone S, et al. Value of home blood pressures as predictor of target organ damage in mild arterial hypertension. J Cardiovasc Risk 2002; 9: 123–29.
18. Tsunoda S, Kawano Y, Horio T, Okuda N, Takishita S. Relationship between home blood pressure and longitudinal changes in target organ damage in treated hypertensive patients. Hypertens Res 2002;25: 167–73.
19. Ohkubo T, Imai Y, Tsuji I, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens 1998; 16: 971–75.
20. Bobrie G, Genès N, Vaur L, et al. Is “isolated home” hypertension as opposed to “isolated offi ce” hypertension a sign of greater cardiovascular risk? Arch Intern Med 2001; 161: 2205–11.
21. Asayama K, Ohkubo T, Kikuya M, et al. Use of 2003 European Society of Hypertension-European Society of Cardiology guidelines for predicting stroke using self-measured blood pressure at home: the Ohasama study. Eur Heart J 2005; 26: 2026–31.