CRP levels are more strongly associated with fatal, than with nonfatal CV events
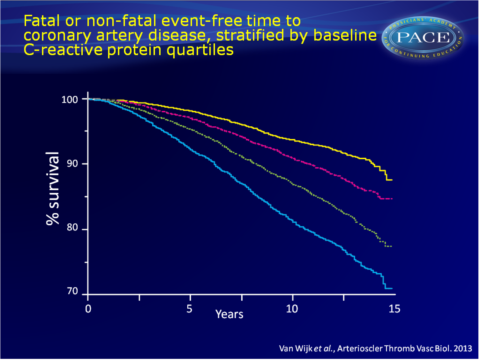
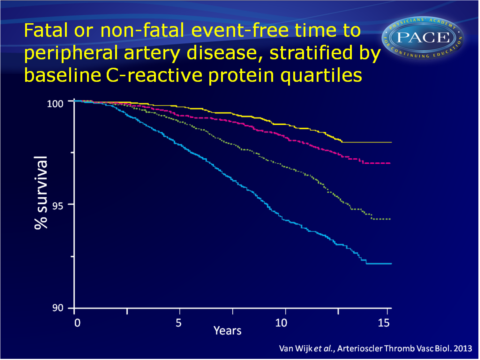
Analysis of EPIC-Norfolk cohort shows independent association of CRP levels with future CAD events, as well as PAD in apparently healthy individuals.
C-Reactive Protein, Fatal and Nonfatal Coronary Artery Disease, Stroke, and Peripheral Artery Disease in the Prospective EPIC-Norfolk Cohort Study.Literature - van Wijk DF, Boekholdt SM, Wareham NJ et al. - Arterioscler Thromb Vasc Biol. 2013 Sep 26
van Wijk DF, Boekholdt SM, Wareham NJ et al.
Arterioscler Thromb Vasc Biol. 2013 Sep 26. [Epub ahead of print]
Background
C-reactive protein (CRP) is an acute phase protein, predominantly produced in the liver. During serious infections or major tissue damage, CRP-plasma levels can rise up to 1000-fold [1]. CRP is present in the atherosclerotic plaque [2]. It has been attributed proatherogenic effects [3-7], and it is now considered a potential causal factor in atherogenesis [7].A causal role has however been debated on the basis of the observation that CRP polymorphisms associated with increased CRP levels were not proportionally associated with in increased risk of coronary artery disease (CAD)[8,9]. A large meta-analysis of individual records of over 160 000 people without a history of vascular disease, showed, however, a strong association between CRP levels and risk of CAD and ischemic stroke [10]. Studies usually considered the sum of both fatal and nonfatal CV events, but CRP may be differentially associated with nonfatal and fatal CAD. Indeed, recently CRP was shown to be more strongly associated with fatal than nonfatal vascular events in the Prospective Study of Pravastatin in the Elderly at Risk (PROSPER) trial [11,12]. Other, experimental studies show that inflammation in general, but also CRP itself, can aggravate myocardial infarction, leading to more severe CV events [13-16].
The authors therefore tested the hypothesis that CRP is more strongly associated with fatal than nonfatal CAD events, strokes and peripheral artery disease (PAD) in the general population, by making use of the EPIC-Norfolk prospective population study.
Main results
- HRs for all fatal CV event were higher as compared with HRs for all nonfatal CV events, although they did not reached the predefined Bonferroni corrected P-value of 0.01.
- Multivariate adjusted HR for 1 mg/L CRP increment for fatal CAD was 1.36 (95%CI: 1.27-1.46) and for nonfatal CAD events was 1.2 (95%CI: 1.15-1.26). These HRs differed significantly (mean difference: 13%, 95%CI: 5.1%-21.9%, P<0.001).
- Multivariate adjusted HR for 1 mg/L CRP increment for fatal stroke and nonfatal stroke did not reach the multiple testing P-value, while unadjusted HR was 1.59 (95%CI; 1.24-2.04) for fatal stroke and 1.38 (95%CI; 1.23-1.52) for nonfatal stroke.
- Multivariate adjusted HR for 1 mg/L CRP increment for fatal PAD not reach the multiple testing P-value, while the adjusted HR for nonfatal PAD events did (HR: 1.36, 95%CI: 1.26-1.48).
- The C-statistic was 0.82 (95%CI: 0.81-0.83, P<0.001) for all combined fatal events (CAD, stroke and PAD) and 0.76 (95%CI: 0.75-0.77, P<0.001) for nonfatal events.
- Using CRP in addition to established CVD risk factors to predict fatal CV events caused 126 individuals to be correctly reclassified into a higher risk category. 112 individuals were incorrectly reclassified into a lower risk category, 1121 individuals were correctly put into a lower category. 897 individuals were incorrectly moved to a higher category.
Net reclassification improvement for fatal events was 2.1% (95%CI: 0.7%-3.5%, P<0.001).
The net reclassification improvement for nonfatal events was similar with 1.9% (95%CI: 0.6%-3.3%, P<0.001). - The Integrated discrimination improvement (IDI) for fatal events was 0.008 (95%CI: 0.006-0.010, P<0.001), and IDI for nonfatal events was 0.003 (95%CI: 0.002-0.004, P<0.001).
Download van wijk ATVB pace.pptx
Conclusion
This study confirms earlier observations that elevated CRP levels are independently associated with increased risk of future CAD events in apparently healthy individuals. Furthermore, it shows that CRP levels are associated with PAD events as well.The association of CRP levels with fatal CAD events is stronger than the one with nonfatal events. This may imply that CRP itself or inflammation in general has a role in promoting more severe CV events, thus yielding a higher propensity of an event to be fatal. This study underscores the need to investigate the efficacy of targeting inflammation for the prevention of CV events.
References
1. Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340:448–454.
2. Zhang YX, Cliff WJ, Schoefl GI, Higgins G. Coronary C-reactive protein distribution: its relation to development of atherosclerosis. Atherosclerosis. 1999;145:375–379.
3. Bisoendial RJ, Birjmohun RS, Akdim F, et al. C-reactive protein elicits white blood cell activation in humans. Am J Med. 2009;122:582.e1–582.e9.
4. van Leuven SI, Birjmohun RS, Franssen R, et al. ApoAI-phosphatidylcholine infusion neutralizes the atherothrombotic effects of C-reactive protein in humans. J Thromb Haemost. 2009;7:347–354.
5. Birjmohun RS, Bisoendial RJ, van Leuven SI, et al. A single bolus infusion of C-reactive protein increases gluconeogenesis and plasma glucose concentration in humans. Metabolism. 2007;56:1576–1582.
6. Bisoendial RJ, Kastelein JJ, Peters SL, et al. Effects of CRP infusion on endothelial function and coagulation in normocholesterolemic and hypercholesterolemic subjects. J Lipid Res. 2007;48:952–960.
7. Bisoendial RJ, Boekholdt SM, Vergeer M et al. C-reactive protein is a mediator of cardiovascular disease. Eur Heart J. 2010;31:2087–2091.
8. Wensley F, Gao P, Burgess S, et al; C Reactive Protein Coronary Heart Disease Genetics Collaboration (CCGC). Association between C reactive protein and coronary heart disease: mendelian randomisation analysis based on individual participant data. BMJ. 2011;342:d548.
9. Zacho J, Tybjaerg-Hansen A, Jensen JS, et al. Genetically elevated C-reactive protein and ischemic vascular disease. N Engl J Med. 2008;359:1897–1908.
10. Kaptoge S, Di Angelantonio E, Lowe G, et al. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet. 2010;375:132–140.
11. Boekholdt SM, Hack CE, Sandhu MS et al. C-reactive protein levels and coronary artery disease incidence and mortality in apparently healthy men and women: the EPIC-Norfolk prospective population study 1993-2003. Atherosclerosis. 2006;187:415–422.
12. Sattar N, Murray HM, Welsh P, et al; Prospective Study of Pravastatin in the Elderly at Risk (PROSPER) Study Group. Are markers of inflammation more strongly associated with risk for fatal than for nonfatal vascular
events? PLoS Med. 2009;6:e1000099.
13. Nijmeijer R, Lagrand WK, Lubbers YT, et al. C-reactive protein activates complement in infarcted
human myocardium. Am J Pathol. 2003;163:269–275.
14. Celik T, Iyisoy A, Yuksel UC et al. The impact of admission C-reactive protein levels on the development of no-reflow phenomenon after primary PCI in patients with acute myocardial infarction: the role of
inflammation. Int J Cardiol. 2009;136:86–88; author reply 88.
15. Mihlan M, Blom AM, Kupreishvili K, et al. Monomeric C-reactive protein modulates classic complement activation on necrotic cells. FASEB J. 2011;25:4198–4210.
16. Griselli M, Herbert J, Hutchinson WL, et al. C-reactive protein and complement are important mediators
of tissue damage in acute myocardial infarction. J Exp Med. 1999;190:1733–1740.
