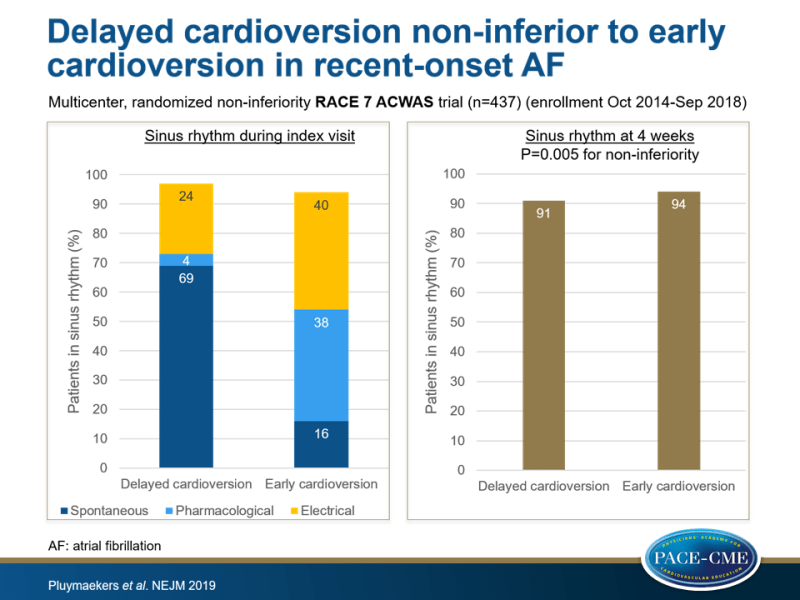
Delayed cardioversion non-inferior to early cardioversion in recent-onset AF
A wait-and-see strategy with rate-control drugs was non-inferior to early pharmacologic or electric conversion in achieving sinus rhythm among patients with recent-onset symptomatic AF.
Early or Delayed Cardioversion in Recent-Onset Atrial FibrillationLiterature - Pluymaekers NAHA, Dudink EAMP, Luermans JGLM et al. - New Eng J Med 2019: DOI: 10.1056/NEJMoa1900353
Introduction and methods
Patients with recent-onset symptomatic atrial fibrillation (AF) are commonly treated immediately with pharmacologic or electrical cardioversion to restore sinus rhythm [1-3]. However, it is unclear whether immediate restoration of sinus rhythm is necessary, since AF often ends spontaneously [4-9]. A wait-and-see strategy consisting of administration of rate-control drugs and delayed cardioversion only if necessary may prevent hospitalization and overtreatment. This non-inferiority trial compared a wait-and-see approach to early cardioversion for achieving sinus rhythm in patients with recent-onset symptomatic AF.
The randomized RACE 7 ACWAS (Rate Control versus Electrical Cardioversion Trial 7–Acute Cardioversion versus Wait and See) trial was conducted in the cardiology departments of 15 hospitals in the Netherlands. Adults (aged ≥18 years) who had presented to the emergency department with hemodynamically stable, symptomatic, recent-onset (<36 hours), first-detected or recurrent AF, without signs of myocardial ischemia or a history of persistent AF (lasting >48 hours) were enrolled from October 2014 through September 2018. After enrollment, 437 participants were randomized 1:1 to either the wait-and-see approach (delayed-cardioversion group) (n=218) or to usual care of early cardioversion (early-cardioversion group) (n=219). The wait-and-see approach consisted of treatment with rate-control drugs, which were given in increasing doses to obtain relief of symptoms and a heart rate of ≤110 beats/min, and delayed cardioversion if needed. Early conversion consisted of pharmacologic cardioversion, preferably with flecainide. In case of contraindications to or previously unsuccessful pharmacologic cardioversion, electrical cardioversion was done.
The primary endpoint was the presence of sinus rhythm on ECG recorded at 4 weeks. At 4 weeks, quality of life (QoL) was assessed using the Atrial Fibrillation Effect on QoL questionnaire (AFEQT), with scores ranging from 0-100 and higher scores indicating a better QoL.
Main results
Delayed vs. early cardioversion and endpoints
- At 4 weeks, ECG-confirmed presence of sinus rhythm was observed in 193 of 212 (91%) patients in the delayed-cardioversion group vs. 202 of 215 (94%) in the early-cardioversion group (between group difference: -2.9 percentage points, 95%CI: -8.2 to 2.2, P=0.005 for non-inferiority).
- CV complications were not significantly different between the two groups (delayed cardioversion: 10 [among which 1 ischemic stroke and 3 acute coronary syndrome (ACS) or unstable angina] vs. early cardioversion: 8 [1 with transient ischemic attack and 3 ACS or unstable angina]). No deaths occurred during follow-up.
- Total median duration of the index visit was 120 (range 60-253) minutes in patients with delayed conversion if needed vs. 158 (range 110-258) minutes in those with early cardioversion (Hodges-Lehman estimated difference between medians: 30 [95%CI: 6-51] minutes).
- Recurrence of AF (based on telemetric ECG recordings, available in 335 patients) within 4 weeks after the index date was seen in 30% (49/164) of patients treated with delayed cardioversion vs. 29% (50/171) of those with early cardioversion.
- The median time until the first episode was 12 (range 3-18) days with delayed cardioversion vs. 8 (range 2-18) days with early cardioversion.
- With delayed cardioversion the mean AFEQT global scores were 72±19, as compared with 73±19 with early cardioversion (difference: -1 point, 95%CI: -5.3 to 4.0). Mean scores on AFEQT subscales were similar between groups for all domains.
Treatment effects of delayed vs. early cardioversion
- In patients with delayed cardioversion, spontaneous conversion to sinus rhythm within 48 hours was observed in 69% of those on rate-control therapy only vs. 28% of those who received delayed cardioversion (9 pharmacologic and 52 electrical). 19% of patients reached rate control without addition of negative dromotropic drugs.
- In the early-cardioversion group, spontaneous conversion to sinus rhythm before initiation of cardioversion was seen in 16% of patients and in 78% after cardioversion (83 pharmacologic and 88 electrical).
Conclusion
This randomized trial showed non-inferiority of a wait-and-see strategy, consisting of treatment with rate-control drugs and later cardioversion if needed, when compared to early cardioversion, in achieving sinus rhythm at 4 weeks after index visit among patients presenting to the emergency department with recent-onset symptomatic AF. In patients with delayed cardioversion, spontaneous conversion was frequently observed, which reduced the need for immediate pharmacologic or electrical cardioversion.
References
1. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2014; 64(21): e1-e76.
2. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 2016; 37: 2893-962.
3. Crijns HJ, Bash LD, Chazelle F, et al. RHYTHM-AF: design of an international registry on cardioversion of atrial fibrillation and characteristics of participating centers. BMC Cardiovasc Disord 2012; 12: 85.
4. Danias PG, Caulfield TA, Weigner MJ, Silverman DI, Manning WJ. Likelihood of spontaneous conversion of atrial fibrillation to sinus rhythm. J Am Coll Cardiol 1998; 31: 588-92.
5. Lindberg S, Hansen S, Nielsen T. Spontaneous conversion of first onset atrial fibrillation. Intern Med J 2012; 42: 1195-9.
6. Geleris P, Stavrati A, Afthonidis D, Kirpizidis H, Boudoulas H. Spontaneous conversion to sinus rhythm of recent (within 24 hours) atrial fibrillation. J Cardiol 2001; 37: 103-7.
7. Cotter G, Blatt A, Kaluski E, et al. Conversion of recent onset paroxysmal atrial fibrillation to normal sinus rhythm: the effect of no treatment and high-dose amiodarone: a randomized, placebo-controlled study. Eur Heart J 1999; 20: 1833-42.
8. Decker WW, Smars PA, Vaidyanathan L, et al. A prospective, randomized trial of an emergency department observation unit for acute onset atrial fibrillation. Ann Emerg Med 2008; 52: 322-8.
9. Doyle B, Reeves M. “Wait and see” approach to the emergency department cardioversion of acute atrial fibrillation. Emerg Med Int 2011; 2011: 545023.
