Differential effect of LDL- and HDL-levels on small and large vessel disease and stroke type
Mendelian randomization study suggests that lowering LDL affects large artery atherosclerosis, but not small artery occlusion or cardioembolic stroke, while increasing HDL may benefit small artery disease.
Role of Blood Lipids in the Development of Ischemic Stroke and its Subtypes: A Mendelian Randomization StudyLiterature - Hindy G, Engström G, Larsson SC, et al. - Stroke. 2018;49:820-827
Introduction and methods
LDL-c lowering trials show that statin therapy leads to a risk reduction of first and recurrent ischemic stroke (IS) [1-3]. However, it is unclear whether the same holds true for different IS subtypes, and whether HDL-c and triglycerides (TGs) may be causally involved in the development of IS as well.
This Mendelian Randomization (MR) study investigated the causal relationship of LDL-c, HDL-c, and TGs in the development of IS and its subtypes. The subtypes studied were cardio-embolic, large artery atherosclerosis stroke, and small artery occlusion.
Summary-level data for 185 genome-wide single nucleotide polymorphisms associated with LDL-c, HDL-c, and TGs were obtained from the publicly available genome-wide association study data through the Global Lipids Genetics Consortium, including 188,577 individuals of primarily European ancestry [4]. The summary-level data for IS and its subtypes were obtained from the National Institute of Neurological Disorders and Stroke−Stroke Genetics Network, which includes 16,851 IS cases and 32,473 controls of predominantly European ancestry [5]. Based on the Org 10172 in Acute Stroke Treatment criteria [6], 2,410 cases were large artery atherosclerosis IS, 3,186 were small artery occlusion IS, and 3,427 were cardio-embolic IS cases.
Main results
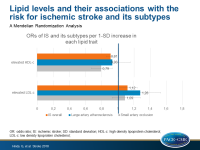
- Genetically predicted LDL-c was associated with higher risk for IS (OR: 1.12; 95%CI: 1.01–1.24; P=0.024; per 1-SD elevation of LDL-c by conventional MR).
- MR-Egger (developed to detect small-study or unbalanced pleiotropy bias) showed a stronger association (OR: 1.22; 95%CI: 1.05–1.43), and did not indicate a pleiotropic bias (P intercept=0.14).
- MR suggested a direct association between genetically elevated LDL-c and large artery atherosclerosis IS (OR: 1.28; 95%CI: 1.07–1.53; P=0.007).
- Genetically predicted LDL-c did not associate with small artery occlusion (OR: 1.21; P=0.303) nor with cardio-embolic stroke.
- Genetically predicted elevations in HDL-c levels were associated with lower risk of small artery occlusion IS (OR: 0.79; 95%CI: 0.67–0.93; P=0.004; per 1-SD elevation of HDL-c). Multivariable MR analyses did not show a significant association between HDL-c and IS, and the MR-Egger estimate showed a null association (OR: 1.01; 95%CI: 0.87–1.18).
- No associations were observed for HDL-c with IS overall (OR: 0.91; P=0.071) or large artery atherosclerosis (OR: 0.93; P=0.480) or cardio-embolic IS.
- Genetically elevated TGs did not associate with IS or any of its subtypes.
Conclusion
This MR study showed that genetically elevated LDL-c levels increase the risk for IS, and in particular the risk of large artery atherosclerosis IS. Genetically predicted elevated HDL-c levels associated with a reduced risk of small artery occlusion IS. Genetically elevated TGs were not associated with a risk reduction of IS or any of its subtypes.
References
1. Baigent C, Blackwell L, Emberson J, et al; Cholesterol Treatment Trialists’ (CTT) Collaboration. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–1681.
2. Amarenco P, Bogousslavsky J, Callahan A 3rd, et al; Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355:549–559.
3. Hosomi N, Nagai Y, Kohriyama T, et al; J-STARS Collaborators. The Japan Statin Treatment Against Recurrent Stroke (J-STARS): a multicenter, randomized, open-label, parallelgroup study. EBioMedicine. 2015;2:1071–1078.
4. Willer CJ, Schmidt EM, Sengupta S, et al; Global Lipids Genetics Consortium. Discovery and refinement of loci associated with lipid levels. Nat Genet. 2013;45:1274–1283.
5. NINDS Stroke Genetics Network (SiGN), International Stroke Genetics Consortium (ISGC). Loci associated with ischaemic stroke and its subtypes (SiGN): a genome-wide association study. Lancet Neurol. 2016;15:174–184.
6. Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24:35–41.