Effect of statin and exercise on mortality
05/12/2012
Lancet, Nov 2012 . Combined effects of fitness and statin treatment on all-cause mortality assessed in prospective cohort study. Statin treatment and exercise lowers mortality risk substantially more than either alone.
Interactive effects of fitness and statin treatment on mortality risk in veterans with dyslipidemia: a cohort study.Literature - Kokkinos PF. et al. Lancet 2012; DOI:10.1016/S0140-6736(12)61426-3
Kokkinos PF, Faselis C, Myers J, et al.
Lancet 2012; DOI:10.1016/S0140-6736(12)61426-3.
Statin treatment substantially reduces morbidity and mortality in patients with coronary heart disease [1-3]. Also people at risk for cardiovascular disease may benefit from statin treatment [4-7]. Lifestyle changes are also important to reduce cardiovascular risk [8,9]. Little data are available on the combined health effects of fitness and statin treatment. This study assessed both the separate and combined effects of statin treatment and exercise capacity on all-cause mortality risk in dyslipidaemic veterans. Data from 10,043 people with dyslipidemia treated at 2 Veterans Affairs Medical Centers were analyzed; participants were followed for a median of 10 years, during which time nearly a quarter of them died.
“The undervaluation of physical activity in clinical practice is unacceptable. Prescription of physical activity should be placed on a par with drug prescription. The cost of becoming physically active is lower than that of buying drugs, and moderate intensity physical activity has fewer side effects. Unlike statins, physical activity should be part of everyday life."
2. Pedersen TR, Olsson AG, Faergeman O, et al. Lipoprotein changes and reduction in the incidence of major coronary heart disease events in the Scandinavian Simvastatin Survival Study (4S). Circulation 1998;97: 1453–60.
3. Sacks FM, Moye LA, Davis BR, et al. Relationship between plasma LDL concentrations during treatment with pravastatin and recurrent coronary events in the Cholesterol and Recurrent Events trial. Circulation 1998; 97: 1446–52.
4. Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90 056 participants in 14 randomised trials of statins. Lancet 2005; 366: 1267–78.
5. Ray KK, Seshasai SR, Erqou S, et al. Statins and all-cause mortality in high-risk primary prevention: a meta-analysis of 11 randomized controlled trials involving 65,229 participants. Arch Intern Med 2010;170: 1024–31.
6. Taylor F, Ward K, Moore TH, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev 2011; CD004816.
7. Thavendiranathan P, Bagai A, Brookhart MA, Choudhry NK. Primary prevention of cardiovascular diseases with statin therapy: a meta-analysis of randomized controlled trials. Arch Intern Med 2006;166: 2307–13.
8. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the Third Report of The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 2001; 285: 2486–97.
9. Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation 2004; 110: 227–39.
10. Hallal PC and Lee IM. Prescription of physical activity: An undervalued intervention. Lancet 2012; DOI:10.1016/S0140-6736(12)61804-2.
Background
Statins are commonly prescribed for management of dyslipidaemia and cardiovascular disease. Increased fitness is also associated with low mortality and is recommended as an essential part of promoting health. However, little information exists about the combined effects of fitness and statin treatment on all-cause mortality. We assessed the combined effects of statin treatment and fitness on all-cause mortality risk.
Methods
In this prospective cohort study, we included dyslipidaemic veterans from Veterans Affairs Medical Centers in Palo Alto, CA, and Washington DC, USA, who had had an exercise tolerance test between 1986, and 2011. We assigned participants to one of four fitness categories based on peak metabolic equivalents (MET) achieved during exercise test and eight categories based on fitness status and statin treatment. The primary endpoint was all-cause mortality adjusted for age, body-mass index, ethnic origin, sex, history of cardiovascular disease, cardiovascular drugs, and cardiovascular risk factors. We assessed mortality from Veteran’s Affairs’ records on Dec 31, 2011. We compared groups with Cox proportional hazard model.
Findings
We assessed 10 043 participants (mean age 58•8 years, SD 10•9 years). During a median follow-up of 10•0 years (IQR 6•0–14•2), 2318 patients died, with an average yearly mortality rate of 22 deaths per 1000 person-years. Mortality risk was 18•5% (935/5046) in people taking statins versus 27•7% (1386/4997) in those not taking statins (p<0•0001). In patients who took statins, mortality risk decreased as fitness increased; for highly fi t individuals (>9 MET; n=694), the hazard ratio (HR) was 0•30 (95% CI 0•21–0•41; p<0•0001) compared with least fi t (≤5 METs) patients (HR 1; n=1060). For those not treated with statins, the HR for least fi t participants (n=1024) was 1•35 (95% CI 1•17–1•54; p<0•0001) and progressively decreased to 0•53 (95% CI 0•44–0•65; p<0•0001) for those in the highest fitness category (n=1498).
Interpretation
Statin treatment and increased fitness are independently associated with low mortality among dyslipidaemic individuals. The combination of statin treatment and increased fitness resulted in substantially lower mortality risk than either alone, reinforcing the importance of physical activity for individuals with dyslipidaemia.
Lancet 2012; DOI:10.1016/S0140-6736(12)61426-3.
Background
Statin treatment substantially reduces morbidity and mortality in patients with coronary heart disease [1-3]. Also people at risk for cardiovascular disease may benefit from statin treatment [4-7]. Lifestyle changes are also important to reduce cardiovascular risk [8,9]. Little data are available on the combined health effects of fitness and statin treatment. This study assessed both the separate and combined effects of statin treatment and exercise capacity on all-cause mortality risk in dyslipidaemic veterans. Data from 10,043 people with dyslipidemia treated at 2 Veterans Affairs Medical Centers were analyzed; participants were followed for a median of 10 years, during which time nearly a quarter of them died.
Main results
- Patients who took statins and were physically fit had as much as a 70% reduction in the risk of dying during the follow-up period as compared with the least physically fit patients who were taking statins (P<0.0001).
- Physical fitness also had an independent effect on mortality risk among patients who were not taking statins, reducing the likelihood of death during follow-up by as much as 47% (P<0.0001).
Conclusion
The combination of statin treatment and a sufficiently high exercise capacity lowers mortality risk substantially more than either alone. This finding suggests that improved fitness is an attractive adjunct treatment to statins or an alternative when statins cannot be taken.
Editorial comment [10]
“The undervaluation of physical activity in clinical practice is unacceptable. Prescription of physical activity should be placed on a par with drug prescription. The cost of becoming physically active is lower than that of buying drugs, and moderate intensity physical activity has fewer side effects. Unlike statins, physical activity should be part of everyday life."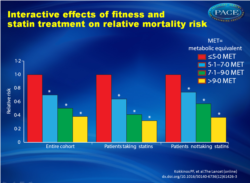 Figure 1: Relative mortality risk by fitness category*Significantly different from reference group. MET=metabolic equivalent. |
References
1. West of Scotland Coronary Prevention Study Group. Influence of pravastatin and plasma lipids on clinical events in the West of Scotland Coronary Prevention Study (WOSCOPS). Circulation 1998; 97: 1440–45.2. Pedersen TR, Olsson AG, Faergeman O, et al. Lipoprotein changes and reduction in the incidence of major coronary heart disease events in the Scandinavian Simvastatin Survival Study (4S). Circulation 1998;97: 1453–60.
3. Sacks FM, Moye LA, Davis BR, et al. Relationship between plasma LDL concentrations during treatment with pravastatin and recurrent coronary events in the Cholesterol and Recurrent Events trial. Circulation 1998; 97: 1446–52.
4. Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90 056 participants in 14 randomised trials of statins. Lancet 2005; 366: 1267–78.
5. Ray KK, Seshasai SR, Erqou S, et al. Statins and all-cause mortality in high-risk primary prevention: a meta-analysis of 11 randomized controlled trials involving 65,229 participants. Arch Intern Med 2010;170: 1024–31.
6. Taylor F, Ward K, Moore TH, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev 2011; CD004816.
7. Thavendiranathan P, Bagai A, Brookhart MA, Choudhry NK. Primary prevention of cardiovascular diseases with statin therapy: a meta-analysis of randomized controlled trials. Arch Intern Med 2006;166: 2307–13.
8. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the Third Report of The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 2001; 285: 2486–97.
9. Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation 2004; 110: 227–39.
10. Hallal PC and Lee IM. Prescription of physical activity: An undervalued intervention. Lancet 2012; DOI:10.1016/S0140-6736(12)61804-2.
Abstract
BackgroundStatins are commonly prescribed for management of dyslipidaemia and cardiovascular disease. Increased fitness is also associated with low mortality and is recommended as an essential part of promoting health. However, little information exists about the combined effects of fitness and statin treatment on all-cause mortality. We assessed the combined effects of statin treatment and fitness on all-cause mortality risk.
Methods
In this prospective cohort study, we included dyslipidaemic veterans from Veterans Affairs Medical Centers in Palo Alto, CA, and Washington DC, USA, who had had an exercise tolerance test between 1986, and 2011. We assigned participants to one of four fitness categories based on peak metabolic equivalents (MET) achieved during exercise test and eight categories based on fitness status and statin treatment. The primary endpoint was all-cause mortality adjusted for age, body-mass index, ethnic origin, sex, history of cardiovascular disease, cardiovascular drugs, and cardiovascular risk factors. We assessed mortality from Veteran’s Affairs’ records on Dec 31, 2011. We compared groups with Cox proportional hazard model.
Findings
We assessed 10 043 participants (mean age 58•8 years, SD 10•9 years). During a median follow-up of 10•0 years (IQR 6•0–14•2), 2318 patients died, with an average yearly mortality rate of 22 deaths per 1000 person-years. Mortality risk was 18•5% (935/5046) in people taking statins versus 27•7% (1386/4997) in those not taking statins (p<0•0001). In patients who took statins, mortality risk decreased as fitness increased; for highly fi t individuals (>9 MET; n=694), the hazard ratio (HR) was 0•30 (95% CI 0•21–0•41; p<0•0001) compared with least fi t (≤5 METs) patients (HR 1; n=1060). For those not treated with statins, the HR for least fi t participants (n=1024) was 1•35 (95% CI 1•17–1•54; p<0•0001) and progressively decreased to 0•53 (95% CI 0•44–0•65; p<0•0001) for those in the highest fitness category (n=1498).
Interpretation
Statin treatment and increased fitness are independently associated with low mortality among dyslipidaemic individuals. The combination of statin treatment and increased fitness resulted in substantially lower mortality risk than either alone, reinforcing the importance of physical activity for individuals with dyslipidaemia.
