Effect of vitamin D on lipid levels
02/07/2012
In this study, a cross-sectional and longitudinal analysis was performed to assess the relationship between 25(OH)D and blood lipids.
Vitamin D May Not Improve Lipid Levels: A Serial Clinical Laboratory Data Study.Literature - Ponda MP et al, Circulation. 2012 Jun 20.
Ponda MP, Huang XX, Odeh MA, Breslow JL, Kaufman HW.
Circulation. 2012 Jun 20. [Epub ahead of print]
An inverse association between circulating levels of 25(OH)D and cardiovascular risk biomarkers, including an atherogenic lipid profile, was suggested in epidemiologic studies [1,2]. A role for supplementation in modifying cardiovascular risk is not well defined. Whether vitamin D status is causally related to disease or merely a marker of health is not clear [3].
In this study, a cross-sectional and longitudinal analysis was performed to assess the relationship between 25(OH)D and blood lipids. From 4.06 million patient records that included simultaneous 25(OH)D and lipid panel tests between 2009 and 2011, 107 811 records had two or more simultaneous 25(OH)D, lipid panels and glucose tests within four and 26 weeks apart. Patients with 25(OH)D concentrations <20 ng/mL were considered vitamin-D deficient while those with levels >30 ng/mL were considered to have optimal levels.
Vitamin-D studies have exploded in the past decade. If read uncritically, the literature would suggest vitamin D appears to be good for almost any condition thinkable and is today the hottest magic cure.
This analysis highlights the difficulties with cross-sectional studies, of which results are often not replicated in prospective studies. Numerous studies have shown that high serum concentrations of 25(OH)D are associated with favourable lipid profiles. However, these associations are not proof of causality. The higher serum 25(OH)D levels in people in good health may be the result and not the cause of good health. Until the results of randomized controlled trials testing vitamin D are available, there is no need to rush recommendations on vitamin-D supplementation based on associations and speculations.
1. Kim DH, Sabour S, Sagar UN, et al. Prevalence of hypovitaminosis D in cardiovascular diseases (from the National Health and Nutrition Examination Survey 2001 to 2004). Am J Cardiol. 2008;102:1540-1544.
2. Forrest KY, Stuhldreher WL. Prevalence and correlates of vitamin D deficiency in US adults. Nutr Res. 2011;31:48-54.
3. Rosen CJ. Clinical practice. Vitamin D insufficiency. N Engl J Med. 2011;364:248-254.
4. Jorde R, Grimnes G. Vitamin D and Lipids: Do We Really Need More Studies? Circulation. 2012 Jun 20. [Epub ahead of print]
Background:
Vitamin D deficiency is highly prevalent and associated with dyslipidemia and cardiovascular disease. The impact is unknown of correcting vitamin D deficiency on blood lipids, strong cardiovascular disease prognostic factors.
Methods and results:
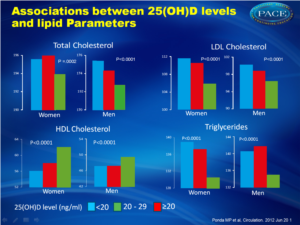
To determine relationships between 25-hydroxyvitamin D levels and lipids, we analyzed 4.06 million de-identified patient laboratory test results from September 2009 through February 2011. We performed a cross-sectional study of this population to determine associations between 25-hydroxyvitamin D levels and lipids across clinically defined strata. We also conducted a retrospective cohort study of vitamin D deficient patients to investigate how changes in 25-hydroxyvitamin D levels relate to changes in lipid levels. After exclusions, 108,711 patients with serial testing were selected for cross-sectional analysis. Compared to vitamin D deficient patients (<20 ng/ml), those with optimal levels (≥30 ng/ml) had lower mean total cholesterol (-1.9 mg/dl [95% CI (-1.2, -2.7 mg/dl)]; p <.0001), lower LDL cholesterol (-5.2 mg/dl [95% CI (-4.5, -5.8 mg/dl)]; p <.0001), higher HDL cholesterol (4.8 mg/dl [95% CI (4.5, 5.0 mg/dl)]; p <.0001), and lower triglycerides (-7.5 mg/dl [95% CI (-6.2, -8.7 mg/dl)]; p <.0001). For the retrospective cohort analysis, raising vitamin D levels from <20 ng/ml to ≥30 ng/ml (n = 6,260), compared to those remaining <20 ng/ml (n = 2,332), was associated with a mean increase in total cholesterol (0.77 mg/dl [95% CI (0.18, 1.36 mg/dl)]; p = .01) and HDL cholesterol (0.42 mg/dl [95% CI (0.08, 0.76 mg/dl)]; p = 0.02), but non-significant changes in LDL cholesterol (0.32 mg/dl [95% CI (-0.01, 0.66 mg/dl)]; p = .06) and triglycerides (0.04 mg/dl [95% CI (-2.16, 2.23 mg/dl)]; p = .97)
Conclusions:
While vitamin D deficiency is associated with an unfavorable lipid profile in cross-sectional analyses, correcting for a deficiency might not translate into clinically meaningful changes in lipid concentrations, although data from intervention trials is required to confirm these findings.
Circulation. 2012 Jun 20. [Epub ahead of print]
Background
An inverse association between circulating levels of 25(OH)D and cardiovascular risk biomarkers, including an atherogenic lipid profile, was suggested in epidemiologic studies [1,2]. A role for supplementation in modifying cardiovascular risk is not well defined. Whether vitamin D status is causally related to disease or merely a marker of health is not clear [3].In this study, a cross-sectional and longitudinal analysis was performed to assess the relationship between 25(OH)D and blood lipids. From 4.06 million patient records that included simultaneous 25(OH)D and lipid panel tests between 2009 and 2011, 107 811 records had two or more simultaneous 25(OH)D, lipid panels and glucose tests within four and 26 weeks apart. Patients with 25(OH)D concentrations <20 ng/mL were considered vitamin-D deficient while those with levels >30 ng/mL were considered to have optimal levels.
Main results
- Patients with optimal levels of vitamin D had total cholesterol levels 1.9 mg/dL lower than patients who were vitamin-D deficient [95% CI (-1.2, -2.7 mg/dl)]; p <.0001).
- LDL-cholesterol levels were 5.2 mg/dL[ 95% CI (-4.5, -5.8 mg/dl)]; p <.0001) and triglyceride levels were 7.5 mg/dL [95% CI (-6.2, -8.7 mg/dl)]; p<.0001) lower among patients with optimal vitamin-D levels , while HDL-cholesterol levels were 4.8 mg/dL higher [95% CI (4.5, 5.0 mg/dl)]; p <.0001).
- Patients who raised their vitamin-D levels into the optimal range had a mean 0.77-mg/dL increase in total cholesterol [95% CI (0.18, 1.36 mg/dl)]; p = .01) and nonsignificant changes in their LDL-cholesterol and triglyceride levels. HDL cholesterol was increased 0.42 mg/dL [95% CI (0.08, 0.76 mg/dl)]; p = 0.02).
Conclusion
Correcting for vitamin-D deficiency with dietary supplements might not translate into clinically meaningful changes in lipid concentrations. This might mean that vitamin-D status is a surrogate marker of health and that vitamin D might simply have no effect on lipid metabolism. Another explanation is that dyslipidemia might be responsible for the low vitamin-D levels and not the other way around.
Editorial comment [4]
Vitamin-D studies have exploded in the past decade. If read uncritically, the literature would suggest vitamin D appears to be good for almost any condition thinkable and is today the hottest magic cure.This analysis highlights the difficulties with cross-sectional studies, of which results are often not replicated in prospective studies. Numerous studies have shown that high serum concentrations of 25(OH)D are associated with favourable lipid profiles. However, these associations are not proof of causality. The higher serum 25(OH)D levels in people in good health may be the result and not the cause of good health. Until the results of randomized controlled trials testing vitamin D are available, there is no need to rush recommendations on vitamin-D supplementation based on associations and speculations.
References
1. Kim DH, Sabour S, Sagar UN, et al. Prevalence of hypovitaminosis D in cardiovascular diseases (from the National Health and Nutrition Examination Survey 2001 to 2004). Am J Cardiol. 2008;102:1540-1544.2. Forrest KY, Stuhldreher WL. Prevalence and correlates of vitamin D deficiency in US adults. Nutr Res. 2011;31:48-54.
3. Rosen CJ. Clinical practice. Vitamin D insufficiency. N Engl J Med. 2011;364:248-254.
4. Jorde R, Grimnes G. Vitamin D and Lipids: Do We Really Need More Studies? Circulation. 2012 Jun 20. [Epub ahead of print]
Abstract
Background:Vitamin D deficiency is highly prevalent and associated with dyslipidemia and cardiovascular disease. The impact is unknown of correcting vitamin D deficiency on blood lipids, strong cardiovascular disease prognostic factors.
Methods and results:
To determine relationships between 25-hydroxyvitamin D levels and lipids, we analyzed 4.06 million de-identified patient laboratory test results from September 2009 through February 2011. We performed a cross-sectional study of this population to determine associations between 25-hydroxyvitamin D levels and lipids across clinically defined strata. We also conducted a retrospective cohort study of vitamin D deficient patients to investigate how changes in 25-hydroxyvitamin D levels relate to changes in lipid levels. After exclusions, 108,711 patients with serial testing were selected for cross-sectional analysis. Compared to vitamin D deficient patients (<20 ng/ml), those with optimal levels (≥30 ng/ml) had lower mean total cholesterol (-1.9 mg/dl [95% CI (-1.2, -2.7 mg/dl)]; p <.0001), lower LDL cholesterol (-5.2 mg/dl [95% CI (-4.5, -5.8 mg/dl)]; p <.0001), higher HDL cholesterol (4.8 mg/dl [95% CI (4.5, 5.0 mg/dl)]; p <.0001), and lower triglycerides (-7.5 mg/dl [95% CI (-6.2, -8.7 mg/dl)]; p <.0001). For the retrospective cohort analysis, raising vitamin D levels from <20 ng/ml to ≥30 ng/ml (n = 6,260), compared to those remaining <20 ng/ml (n = 2,332), was associated with a mean increase in total cholesterol (0.77 mg/dl [95% CI (0.18, 1.36 mg/dl)]; p = .01) and HDL cholesterol (0.42 mg/dl [95% CI (0.08, 0.76 mg/dl)]; p = 0.02), but non-significant changes in LDL cholesterol (0.32 mg/dl [95% CI (-0.01, 0.66 mg/dl)]; p = .06) and triglycerides (0.04 mg/dl [95% CI (-2.16, 2.23 mg/dl)]; p = .97)
Conclusions:
While vitamin D deficiency is associated with an unfavorable lipid profile in cross-sectional analyses, correcting for a deficiency might not translate into clinically meaningful changes in lipid concentrations, although data from intervention trials is required to confirm these findings.