Effects of hypertensive target organ damage on vascular events and mortality
07/02/2013
J Hypertens. 2013 Jan. This study evaluates the separate and combined effects of impaired renal function, albuminuria and left-ventricular hypertrophy (LVH) on the occurrence of vascular events and mortality in patients with vascular disease.
AbstractLiterature -
Hypertensive target organ damage and the risk for vascular events and all-cause mortality in patients with vascular disease.
Vernooij JW, Van Der Graaf Y, Nathoe HM, et al.J Hypertens. 2013 Jan 8. [Epub ahead of print]
Background
Impaired renal function, albuminuria, and/or left ventricular hypertrophy (LVH) are manifestations of hypertensive target organ damage and are each associated with increased risk for vascular events and for mortality [1,2]. Although these manifestations of target organ damage are most often the result of hypertension, the exact pathophysiological mechanisms by which they contribute to increased vascular risk are poorly understood. In healthy individuals the presence of subclinical target organ damage, including LVH and albuminuria, as well as the number of organs damaged, was associated with increased cardiovascular risk independently of the Systematic COronary Risk Evaluation (SCORE risk) algorithm [3]. It is unknown whether combined presence of hypertensive target organ damage confers higher vascular risk compared to single presence. This study evaluates the separate and combined effects of impaired renal function, albuminuria and left-ventricular hypertrophy (LVH) on the occurrence of vascular events and mortality in patients with vascular disease. The addition of IMT to the other measurements of hypertensive target organ damage in prevalence and risk for vascular events and mortality was evaluated. The patients included in this study originated from the Second Manifestations of ARTerial disease (SMART) study [4]. A cohort of patients with vascular diseases (n=4319) was followed (median 4.4 years) for the occurrence of vascular events (stroke, myocardial infarction, vascular death) and mortality.
Main results
- 34% had at least one manifestation of target organ damage. The combined presence of at least two manifestations of hypertensive target organ damage was found in 345 patients (8%). All three target organ damages were present in 47 patients (1%).
- Albuminuria was most prevalent (18%), followed by impaired renal function (15%) and LVH (11%).
- The risk for vascular events was hazard ratio 1.5 [95% confidence interval (CI) 1.2–1.9] for presence of one hypertensive target organ damage and hazard ratio 3.8 (95% CI 2.3–6.3) for three manifestations of hypertensive target organ damage (adjusted for age, sex).
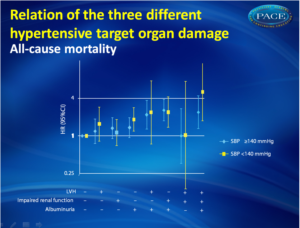
- For mortality this risk was hazard ratio 1.4 (95% CI 1.1–1.7) and hazard ratio 3.2 (95% CI 1.9–5.2).
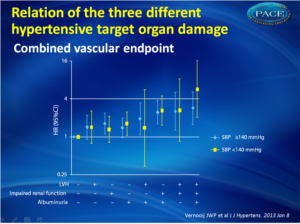
- Presence or absence of elevated blood pressure did not affect the relation between target organ damage and combined vascular endpoints and mortality. (fig. 1)
Conclusion
The single and combined presence of impaired renal function, albuminuria, and LVH is highly prevalent in patients with clinically manifest vascular disease and confers independent and additive risks for the combined vascular endpoints and mortality. Routine measurement of hypertensive target organ damage identifies patients at the highest risk and may direct treatment of blood pressure.References
1. Vakili BA, Okin PM, Devereux RB. Prognostic implications of left ventricular hypertrophy. Am Heart J 2001; 141:334–341.2. Vlek AL, van der Graaf Y, Spiering W, et al. Cardiovascular events and all-cause mortality by albuminuria and decreased glomerular filtration rate in patients with vascular disease. J Intern Med 2008; 264:351–360.
3. Sehestedt T, Jeppesen J, Hansen TW, et al. Risk prediction is improved by adding markers of subclinical organ damage to SCORE. Eur Heart J 2010; 31:883–891.
4. Simons PC, Algra A, van de Laak MF, et al. Second manifestations of ARTerial disease (SMART) study: rationale and design. Eur J Epidemiol 1999; 15:773–781.
Objective:
Presence of hypertensive target organ damage is related to increased vascular risk and mortality. Whether combined presence of hypertensive target organ damage confers higher vascular risk compared to single presence is unknown. This study evaluates the separate and combined effects of impaired renal function [estimated glomerular filtration rate (eGFR) ≤60 ml/min per 1.73 m], albuminuria (albumin/creatinine-ratio men ≥2.5 mg/mmol, women ≥3.5 mg/mmol) and left-ventricular hypertrophy (LVH) (Sokolow-Lyon and/or Cornell-voltage criterion) on the occurrence of vascular events and mortality in patients with vascular disease (coronary artery disease, cerebrovascular disease, and peripheral arterial disease).
Methods and results:
A cohort of patients with vascular diseases (n = 4319) was followed (median 4.4 years) for the occurrence of vascular events (stroke, myocardial infarction, vascular death) and mortality. LVH was present in 11%, impaired renal function in 15%, and albuminuria in 18%. Presence of at least two hypertensive target organ damage was prevalent in 8%. The risk for vascular events was hazard ratio 1.5 [95% confidence interval (CI) 1.2-1.9] for presence of one hypertensive target organ damage and hazard ratio 3.8 (95% CI 2.3-6.3) for three manifestations of hypertensive target organ damage (adjusted for age, sex). For mortality this was hazard ratio 1.4 (95% CI 1.1-1.7) and hazard ratio 3.2 (95% CI 1.9-5.2). Hazard ratios for single presence of different types of organ damage were comparable and independent of the presence of hypertension.
Conclusions:
Impaired renal function, albuminuria, and LVH are prevalent in patients with vascular disease and confer independent and additive risk for vascular events and mortality. Measurement of hypertensive target organ damage in patients with vascular disease identifies patients at very high risk and may have treatment implications.