Even normotensive young blacks have a higher risk of hypertension than whites
Black individuals have a significantly higher risk for hypertension compared with whites, from young adulthood through middle age, irrespective of BP before the age of 30 years.
Cumulative Incidence of Hypertension by 55 Years of Age in Blacks and Whites: The CARDIA StudyLiterature - Thomas SJ, Booth JN, Dai C, et al. - J Am Heart Assoc. 2018;7:e007988
Introduction and methods
Existing data show that blacks have higher blood pressure (BP) levels, an increased risk for hypertension, and a higher prevalence of hypertension compared with whites. Limited longitudinal data are available, however, to quantify the cumulative incidence (CI) of hypertension from young adulthood through middle age [1-3].
In this analysis of the Coronary Artery Risk Development in Young Adults (CARDIA) study [4], the CI of hypertension was assessed in black and white adults aged 18-30 years, who have been followed until the age of 55. Moreover, risk factors associated with a higher risk for hypertension were identified, which may prove to be meaningful goals for primordial prevention.
In CARDIA, 5,115 black and white individuals aged 18-30 years were enrolled between 1985 and 1986. For the current analysis, those with valid clinic BP measurements at baseline and during at least 1 follow-up examination were included, those who had systolic BP (SBP)<130 mmHg, diastolic BP (DBP) <80 mmHg, were not receiving antihypertensive treatment, and had no diagnosis of hypertension at the time of enrollment (N=3,890). Data on other risk factors were self-reported. The follow-up lasted 30 years. Incident hypertension was defined by the first visit with a mean SBP ≥130 mmHg, or a mean DBP ≥80 mmHg, or self-reported use of antihypertensive treatment.
Main results
- At baseline, participants had a mean age of 24.7 years, 42.4% were men, 49.3% were black, and 52.4% developed hypertension (51.4% had SBP ≥130 mmHg or DBP ≥80 mmHg, but were not taking antihypertensive treatment).
- Blacks had higher mean BMI (24.8±5.1) than whites (23.3±3.7, P<0.001), and higher mean SBP (108.8±8.9 vs 106.8±9.1 mmHg).
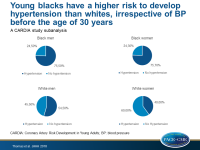
- At the age of 55, the CI of hypertension was 75.5% in black men, 75.7% in black women, 54.5% in white men, and 40.0% in white women.
- The subgroups with the highest CI of hypertension at 55 years of age were: blacks with SBP/DBP 120-129/75-79 mmHg (CI: 88.1%), blacks with SBP/DBP 110-119/70-74 mmHg (CI: 79.7%), whites with SBP/DBP 120-129/75-79 mmHg (CI: 71.5%), blacks with SBP/DBP <110/70 mmHg (CI: 64.0%).
- The subgroups with the lowest CI of hypertension at 55 years of age were: whites with SBP/DBP of 110-119/70-74 mmHg (CI: 52.6%), whites with SBP/DBP <110/70 mmHg (CI: 32.7%).
- After multivariable adjustment, the risk for hypertension was higher in blacks compared with whites, regardless of baseline BP level (Pinteraction >0.2):
- <110 and 70 mmHg at baseline: HR:1.97, 95%Confidence Interval: 1.65-2.35
- 110 to 119/70 to 74 mmHg at baseline HR:1.80, 95% Confidence Interval: 1.52-2.14
- 120 to 129/75 to 79 mmHg at baseline HR:1.59, 95% Confidence Interval: 1.31-1.93
- Both in blacks and whites, family history of hypertension, higher BMI, serum uric acid, and baseline SBP/DBP categories were associated with an increased risk for hypertension, whereas a higher DASH diet adherence score was associated with a lower risk for hypertension.
- High levels of physical activity and female gender were associated with a lower risk for hypertension in whites only, and older age was only associated with a higher risk for hypertension in blacks.
Conclusion
Black individuals have a significantly higher risk of developing hypertension by the age of 55 compared with whites, from young adulthood through middle age, even in individuals with SBP/DBP <110/70 mmHg in young adulthood. The differences in incident hypertension emerged before 30 years of age, suggesting that early prevention should be considered for blacks at a young age.
Editorial comment
In the editorial article, Brent [5] emphasizes the need and value of lifestyle interventions early in life, in order to decrease the risk for hypertension in black individuals. He also underlines that the 2017 ACC/AHA Hypertension Guideline recommendation to start antihypertensive medication for stage 1 hypertension may be more beneficial in blacks than in whites. He concludes: ‘Cost-effective and highly scalable approaches to healthy lifestyle patterns are urgently needed, especially in younger blacks. Because many blacks ≤55 years of age have 10-year CVD risk ≥10% or higher, effective pharmacotherapy should attenuate progression to more severe hypertension and potentially reduce cardiovascular events. Novel approaches to hypertension prevention, detection, treatment, and control may be required to improve health equity, given large racial differences in the age of onset, prevalence, and severity of hypertension.’
References
1. Hertz RP, Unger AN, Cornell JA, et al. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165:2098–2104.
2. Cutler JA, Sorlie PD, Wolz M, et al. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52:818–827.
3. Guo F, He D, Zhang W, et al. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol. 2012;60:599–606.
4. Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116.
5. Egan BM. Defining Hypertension by Blood Pressure 130/80 mmHg Leads to an Impressive Burden of Hypertension in Young and Middle-Aged Black Adults: Follow-Up in the CARDIA Study. J Am Heart Assoc. 2018;7:e009971.