Favorable net clinical benefit with P2Y12 inhibitor in addition to aspirin in CAD patients with T2DM and prior PCI
ESC 2019 Addition of ticagrelor to aspirin resulted in a reduction of CV outcomes in CAD patients with diabetes, but at the expense of increased bleeding. Net clinical benefit was favorable in those with previous PCI.
THEMIS: Ticagrelor Added to Aspirin in Patients with Stable Coronary Disease and DiabetesNews - Sep. 1, 2019
Presented at the ESC congress 2019 in Paris, France by: Deepak Bhatt (Newton, MA, USA)
THEMIS-PCI: Ticagrelor Added to Aspirin in Patients with Diabetes and Stable Coronary Artery Disease with a History of Prior Percutaneous Coronary Intervention
Presented at the ESC congress 2019 in Paris, France by: Gabriel Steg (Paris, France)
Introduction and methods
Patients with stable coronary artery disease (CAD) and type 2 diabetes (T2DM) are at increased risk of CV events. The P2Y12 inhibitor ticagrelor, in addition to aspirin, has demonstrated to give benefit in patients with acute coronary syndrome (ACS) and in those with previous myocardial infarction (MI). It is unknown whether CAD patients with T2DM without prior MI or stroke benefit from ticagrelor in combination with aspirin.
THEMIS is a randomized, double-blind, placebo-controlled trial enrolling 19220 T2DM patients ≥50 years with stable CAD (history of PCI, CAD or angiographic stenosis ≥50% in at least 1 coronary artery). Patients were randomized in a 1:1 ratio to receive ticagrelor or placebo, in addition to aspirin. Initially dosing of ticagrelor was 90 mg bid, then 60 mg bid due to insights from the PEGASUS-TIMI 54 trial.
Primary outcome was a composite of CV death, MI and stroke.
A prespecified analysis of THEMIS patients with a history of PCI (and previously treated with DAPT) was undertaken with the hypothesis that this group would have a favorable balance of efficacy and safety.
Main results
Results for the overall study population
- The primary endpoint was reduced in the ticagrelor group compared to the placebo group (event rate at 36 months 6.9% vs. 7,6%, HR: 0.90, 95%CI: 0.81-0.99, P=0.038).
- Ticagrelor treatment resulted in a significant reduction of the secondary outcomes MI and ischemic stroke compared to placebo. Also, outcomes of all-cause death/MI/stroke, all stroke, acute limb ischemia/major amputation, all-cause death/MI/stroke/ALI/major amputation were reduced with ticagrelor compared to placebo.
- Bleeding outcomes were increased with ticagrelor compared to placebo, with significant findings for TIMI major bleeding (HR: 2.32, 95%CI: 1.82-2.94, P<0.001), TIMI major or minor bleeding, TIMI major, minor bleeding or requiring medical attention, PLATO major bleeding, BARC type 5, 4, 3 bleeding, intracranial hemorrhage and traumatic intracranial hemorrhage.
- On-treatment analysis showed that ticagrelor reduced the primary endpoint compared to placebo (HR: 0.81, 95%CI: 0.71-0.92, P=0.01).
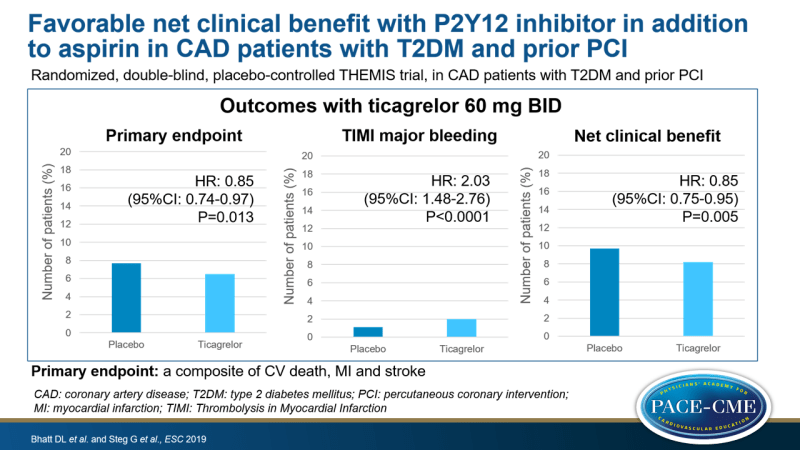
Results for the PCI population
- Use of ticagrelor resulted in a decrease of the primary endpoint compared to placebo (event rate at 36 months: 6.5% vs. 7.7%, HR: 0.85, 95%CI: 0.74-0.97, P=0.013). There was no difference in reduction with ticagrelor in those with previous PCI vs. those without (P-interaction=0.16).
- Secondary endpoints of all-cause death/stroke/MI, all-cause death/MI/stroke/ALI/major amputations, MI, STEMI, and stroke were reduced in the ticagrelor group vs. the placebo group.
- Treatment with ticagrelor resulted in an increase in TIMI major bleeding compared to placebo (HR: 2.03, 95%CI: 1.48-2.76, P<0.0001), as well as BARC type 2, 3, 4 or 5 bleeding.
- Net clinical benefit, the composite of all-cause death, MI, stroke, fatal bleed or ICH, was reduced with ticagrelor compared to placebo (8.2% vs. 9.7% at 36 months, HR: 0.85, 95%CI: 0.75-0.95, P=0.005).
- In those without a history of PCI, there was no net clinical benefit with ticagrelor vs. placebo (HR: 1.06, 95%CI:0.93-1.21). There was a difference in the effect of ticagrelor on net clinical benefit when comparing patients with a history of PCI vs. those without (P-interaction=0.012).
Conclusion
Treatment with ticagrelor, in addition to aspirin, in patients with CAD and T2DM resulted in a reduction of the composite endpoint of CV death, MI and stroke. This benefit, however, was at the expense of an increased risk for major bleeding. In those with previous PCI, ticagrelor treatment resulted in a favorable net clinical benefit.
The combination of long-term ticagrelor and aspirin may be beneficial in selected patients at high risk of ischemic events and low risk of bleeding.
Discussion
In response to a question which other high risk population could benefit from this DAPT therapy, Steg answered that this is likely in those who had a stent, because their bleeding risk is lower and these patients had previously received DAPT therapy.
Recommendations for ticagrelor plus aspirin in patients with CAD and T2DM include patients with a history of PCI and those with a low bleeding risk, according to Bhatt.
- Our reporting is based on the information provided at the ESC congress -
Watch our video about the THEMIS trial