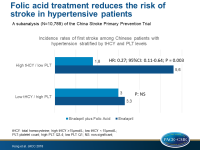
Folic acid treatment reduces the risk of stroke in hypertensive patients
Patients with hypertension with low platelet counts and high total homocysteine levels, which may promote platelet adherence, had the highest risk of first stroke, and this risk was reduced with folic acid treatment.
Platelet Count Affects Efficacy of Folic Acid in Preventing First StrokeLiterature - Kong X, Huang X, Zhao M, et al. - J Am Coll Cardiol 2018;71:2136–46
Introduction and methods
The role of platelets in the pathophysiology of atherosclerosis and atherothrombosis is well understood, however, it is not clear whether platelet count (PLT) is associated with risk of stroke [1]. Low PLT has been linked to endothelial injury, for instance in the presence of elevated total homocysteine levels (tHcy) and as a consequence, higher platelet adherence [2,3]. Moreover, increased tHcy levels is a risk factor for cardiovascular (CV) disease, but there are no relevant data regarding stroke [3,4]. The China Stroke Primary Prevention Trial (CSPPT) did show, however, that folic acid treatment, known to lower tHcy, reduces the risk of first stroke by 21% in hypertensive individuals [5].
This sub-analysis of the CSPPT, therefore prospectively evaluated the association between baseline PLT and tHcy levels and first stroke risk in Chinese hypertensive adults. Moreover, the effects of folic acid administration in these patients was assessed. Out of the 20,702 CSPPT participants, after excluding those without baseline PLT and tHcy measurements, as well as those who were receiving antiplatelet medications, 10,789 patients were eligible for this analysis.
Participants were randomly assigned in a 1:1 ratio to receive either 10 mg enalapril and 0.8 mg folic acid daily (E+FA group), or 10 mg enalapril only (E group). Median follow-up was 4.2 years and the primary outcome was the occurrence of a first nonfatal or fatal stroke (ischemic or hemorrhagic), which occurred 210 times in the E group and 161 times in the E+FA group.
Main results
- In the E group, participants with low PLT (Q1) had the highest risk of first stroke (4.6%) compared to those in the higher PLT quartiles (3.7%).
- In the E+FA group, the stroke incidence was reduced from 4.6% to 1.9% in the low PLT quartile (ARR: 2.7%; RRR: 58; HR: 0.42; 95%CI: 0.26-0.68; P <0.001). The stroke risk reduction in the high PLT quartiles was modest (HR: 0.90; 95%CI: 0.71-1.14; P=0.382).
- In patients with low PLT (Q1) folic acid treatment resulted in a significant reduction in first stroke risk, with HRs ranging from 0.19 to 0.57 across various subgroup analyses. In patients with higher PLT (Q2 to Q4), the efficacy of folic acid was greatly attenuated, with HRs ranging from 0.70 to 1.12.
- In the enalapril group, the lowest incidence rate of first stroke (3.3%) was found in patients with high PLT (Q2 to Q4) and low tHcy (<15 mmol/l), whereas the highest rate (5.6%) was found in those with low PLT (Q1) and high tHcy (≥15 mmol/l).
- Following folic acid treatment, the risk of first stroke was reduced from 5.6% to 1.8% among patients with low PLT and high tHcy, whereas folic acid treatment had no effect on incident stroke among those with high PLT (Q2 to Q4) and low tHcy (3%).
- Using tHcy >15 mmol/l as a cutoff, and compared with the E group, folic acid treatment was most effective and reduced the risk of first stroke by 73% (HR: 0.27; 95%CI: 0.11-0.64; P = 0.003) in patients with high tHcy and low PLT.
Conclusion
In Chinese patients with hypertension, the risk of first stroke varied between subgroups based on PLT and tHcy levels. The subgroup with low PLT and high tHcy at baseline had the highest risk of first stroke over a median of 4.2 years of follow-up, and this risk was reduced by 73% with folic acid treatment. In those with high PLT and low tHcy, folic acid had no effect on reducing the risk of first stroke. If confirmed, these findings can help identify patients at high risk of stroke and who would benefit most from treatment with folic acid treatment.
Editorial comment
In their editorial article, Spence and Hachinski [6] discuss the pathophysiological background of reducing stroke risk with folic acid treatment. tHcy may promote platelet adhesion and cause low platelet counts. Patients with low platelet counts and high tHcy levels may be at higher risk, due to vitamin B12 deficiency. They also emphasize that B vitamins do reduce the risk of stroke, a finding that has been found to be attenuated by renal dysfunction in early trials.
The authors conclude: ‘Recognition that folate reduces the risk of stroke in a jurisdiction where folate fortification does not exist has important implications for prevention of both stroke and dementia. The recent recognition that harm from cyanocobalamin among study participants with renal impairment obscured the benefit of B vitamins in the early studies suggests that methylcobalamin should be used instead of cyanocobalamin. Further studies of folate and methylcobalamin should be carried out for prevention of both stroke and dementia; the findings of Kong et al. provide a strong rationale for doing so.’
References
1. Bigalke B, Schuster A, Sopova K, et al. Platelets in atherothrombosis—diagnostic and prognostic value of platelet activation in patients with atherosclerotic diseases. Curr Vasc Pharmacol 2012;10:589–96.
2. Zhao M, Wang X, He M, et al. Homocysteine and stroke risk: modifying effect of methylenetetrahydrofolate reductase C677T polymorphism and folic acid intervention. Stroke 2017;48: 1183–90.
3. Collaboration HS. Homocysteine and risk of ischemic heart disease and stroke: a meta-analysis. JAMA 2002;288:2015–22.
4. Wald DS, Law M, Morris JK. Homocysteine and cardiovascular disease: evidence on causality from a meta-analysis. BMJ 2002;325:1202.
5. Huo Y, Li J, Qin X, et al. Efficacy of folic acid therapy in primary prevention of stroke among adults with hypertension in China: the CSPPT randomized clinical trial. JAMA 2015;313:1325–35.
6. Spence DJ, and Hachinski V. B Vitamins for Stroke Prevention: Interaction of Low Platelet Count and High Plasma Total Homocysteine. J Am Coll Cardiol 2018;71:2147-8.