Heart failure severity associated with risk of diabetes
Danish nationwide study shows that risk of developing diabetes increases with HF severity, as assessed by prescribed dosage of loop-diuretics.
Association of heart failure severity with risk of diabetes: a Danish nationwide cohort studyLiterature - Demant MN et al., Diabetologia. 2014 - Diabetologia. 2014 May 22
Demant MN, Gislason GH, Køber L, et al.
Diabetologia. 2014 May 22. [Epub ahead of print]
Background
The Framingham Heart Study first reported that diabetes was associated with worsened prognosis in patients with heart failure (HF), nearly 35 years ago [1]. Little improvement has, however, been seen in the prognosis of HF in relation to diabetes despite the availability of more intense glucose-lowering pharmacotherapy.It has been hypothesised that diabetes can be a marker of HF severity rather than a causal risk factor for adverse outcomes. Indeed, chronic HF has been shown to be associated with hyperinsulinaemia and increased insulin resistance, in a severity-dependent matter [2-4]. It had previously been shown that HF patients had a higher risk of developing diabetes after previous myocardial infarction [5].
This nationwide study aimed to investigate whether a relation exists between loop-diuretic dosages, as a proxy for HF severity, and risk of diabetes for patients discharged after first-time HF hospitalisation, and the prognostic effect of developing diabetes in chronic HF. To this extent, four Danish nationwide administrative registers were cross-linked at the individual level (i.e. the Danish National Patient Registry, the Danish Registry of Medicinal Product Statistics, Anatomical Therapeutical Chemical system and the National Population Register). 99.362 Danish citizens of 30 years and older admitted with first-time HF between 1997 and 2010, and alive 90 days after discharge (baseline) were included in this study, excluding those who had claimed prescriptions of hypoglycaemic agents before hospitalisation for HF.
Main results
- 7958 patients (8%) developed diabetes, after a median time to first claimed prescription of a hypoglycaemic agents of 1080 days (IQR: 475-2037).
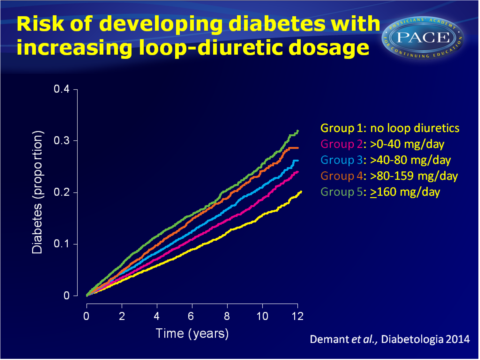
- Patients were divided into 5 groups with increasing prescribed dosage of loop-diuretics at baseline. The proportion of patients who developed diabetes increased with dosage of loop-diuretics. Crude incidence rates for developing diabetes were 1.6 (95%CI: 1.5-1.7), 1.9 (95%CI: 1.5-2.0), 2.3 (95%CI: 2.2-2.4), 2.6 (95%CI: 2.5-2.8) and 3.0 (95%CI: 2.9-3.2) per 100 person-years in groups 1 through 5 respectively.
- In adjusted Cox regression models, HR increased with each next loop-diuretic dosage group, as compared to group 1. HR in group 5 was 2.09 (95%CI: 1.94-2.25).
- In each group, use of renin angiotensin system inhibitors (RASi) attenuated risk of developing diabetes, for instance in group 5, HR without RASi was 1.76 (95%CI: 1.61-19.2), while HR with RASi was 3.02 (95%CI: 2.66-3.43). Use of beta-blockers gave a lower risk of diabetes, similar to RASi.
- HRs were also slightly lower for patients with ischaemic heart disease than for patients without in loop-diuretic dose groups 2 to 5, as compared with group 1.
- 62.565 (63%) of patients died during the study period. The risk of dying was higher in patients who developed diabetes, than in HF patients without diabetes (HR: 1.16, 95%CI: 1.12-1.19). Increasing loop-diuretic dosage groups showed higher risks of dying, up until HR: 1.45 (95%CI: 1.41-1.48) in group 5, as compared to group 1.
Download Demant diabetologia 2014-PACE.pptx
Conclusion
This nationwide study shows that among patients hospitalised for HF, increasing loop-diuretic dosage, as estimated at day 90 after discharge, and used as a proxy for HF severity, is associated with a higher risk of developing diabetes. Thus, this association is not restricted to patients who had experienced a myocardial infarction.Patients who developed diabetes are at higher risk of death than HF patients not developing diabetes. The sickest patients may develop diabetes. Diabetes might thus be a marker of HF severity, as well as being a causal risk factor for mortality in HF cohorts.
This study emphasises the importance of monitoring and treatment of patients with HF to prevent development of diabetes.
Find this article on Pubmed
References
1. Kannel WB, McGee DL (1979) Diabetes and cardiovascular disease. The Framingham study. J Am Med Assoc 241:2035–2038
2. Swan JW, Anker SD, Walton C et al (1997) Insulin resistance in chronic heart failure: relation to severity and etiology of heart failure. J Am Coll Cardiol 30:527–532
3. AlZadjali MA, Godfrey V, Khan F et al (2009) Insulin resistance is highly prevalent and is associated with reduced exercise tolerance in nondiabetic patients with heart failure. J Am Coll Cardiol 53:747–753
4. Nikolaidis LA, Sturzu A, Stolarski C et al (2004) The development of myocardial insulin resistance in conscious dogs with advanced dilated cardiomyopathy. Cardiovasc Res 61:297–306
5. Andersson C, Norgaard ML, Hansen PR et al (2010) Heart failure severity, as determined by loop diuretic dosages, predicts the risk of developing diabetes after myocardial infarction: a nationwide cohort study. Eur J Heart Fail 12:1333–1338
