High dose atorvastatin also beneficial for gum disease
High-dose statin therapy reduced periodontal inflammation, suggestive of a cholesterol-independent beneficial effect of statins on non-arterial inflammation.
High Dose Atorvastatin Reduces Periodontal Inflammation: A Novel Pleiotropic Effect of Statins.Literature - Subramanian S, Emami H, et al. - J Am Coll Cardiol. 2013 Sep 23
Subramanian S, Emami H, Vucic E et al.
J Am Coll Cardiol. 2013 Sep 23. doi: 10.1016/j.jacc.2013.08.1627. [Epub ahead of print]
Background
Periodontal disease (PD) is a common, independent risk factor for atherosclerotic disease [1,2]. Local periodontal inflammation, through pro-inflammatory cytokine release, has been proposed to lead to systemic inflammation, as measured by CRP, TNA-α, IL-6 and other biomarkers. This is one of the postulated pathogenic mechanisms linkin PD and cardiovascular (CV) disease [3-5]. Increased levels of circulating inflammatory mediators can then promote inflammatory activity within atherosclerotic plaques [6,7].Local treatment of PD has been shown to reduce systemic inflammation in patients with a history of CV events [8]. No definitive evidence exists, however, that treatment of periodontal disease decreases CV disease progression or CV events.
18F-Flurodeoxyglucose positron emission tomography (FDG-PET) imaging provides a non-invasive measure of inflammation, also of inflammatory activity within atherosclerotic plaques. The authors have previously shown that periodontal inflammation correlates with carotid artery inflammation [9]. Others have recently demonstrated that periodontal FDG uptake correlates with PD severity as measured by alveolar bone loss [10].
Retrospective epidemiologic studies have shown that statin therapy is associated with reduced severity of periodontitis [11-14]. Furthermore, it was shown recently that a combination of statins and standard local periodontal treatment was more effective than the local treatment alone [15].
This double-blind, randomised, active-comparator study aimed to study the direct anti-inflammatory actions of statins in periodontal tissue, by using FDG-PET/CT imaging to test if high-dose atorvastatin treatment lowers periodontal disease activity, similar to its action on atherosclerotic plaque activity. 71 subjects completed the study, and for 59 of those periodontal tissue images were available.
Main results
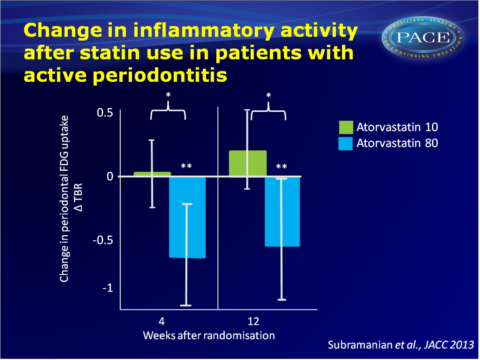
- Mean periodontal FDG uptake was significantly reduced in the entire cohort after 12 weeks of treatment with high (80 mg) vs. low (10 mg) dose atorvastatin (mean Target-to-background ratio (TBR): -0.29 + 0.85 (SD) vs. 0.13 + 0.68, P0.04). The effect of high dose atorvastatin on PD activity remained statistically significant after correction for several possible confounders.
- The effect of high-dose statin treatment was more pronounced in subjects with imaging evidence of periodontal disease at baseline; in individuals with active periodontitis there were clear differences between the two statin doses (change TBR= -0.52 + 0.94 vs. 0.22 + 0.79, P=0.01). The difference between groups was already evident after 4 weeks.
- Baseline FDG uptake (TBR) in periodontal tissue correlated with baseline carotid plaque TBR. Also, after 12 weeks of statin treatment, changes in periodontal inflammation correlated with changes in carotid inflammation.
- Baseline PD activity (periodontal TBR) was inversely correlated with baseline HDL concentration (r= -0.35, P=0.007), but did not correlate with baseline CRP or LDL levels. Changes in PD activity did not correlate with changes in CRP, LDL or HDL.
Download subramanian JACC 2013 pace.pptx
Conclusion
Twelve weeks of high-dose statin therapy significantly reduces periodontal inflammation. The reduction in PD activity was already seen after 4 weeks of atorvastatin treatment and correlated with changes in FDG uptake in the carotid wall.It has previously been suggested that statins have effects beyond their lipid-lowering actions. This study provides evidence for a cholesterol-independent, or ‘pleiotropic’ effect of statins, namely reduction in non-arterial inflammation. The authors further postulate that a reduction in local periodontal inflammation may also exert beneficial effects on the systemic arterial milieu, through a reduced release of pro-inflammatory mediators from the periodontal tissue, into the systemic circulation.
References
1. Genco R, Offenbacher S, Beck J. Periodontal disease and cardiovascular disease: epidemiology and possible mechanisms. J Am Dent Assoc 2002;133 Suppl:14S-22S.
2. Beck J, Garcia R, Heiss G, et al. Periodontal disease and cardiovascular disease. J Periodontol 1996;67:1123-37.
3. Linden GJ, McClean K, Young I, et al. Persistently raised C-reactive protein levels are associated with advanced periodontal disease. J Clin Periodontol 2008;35:741-7.
4. Noack B, Genco RJ, Trevisan M, et al. Periodontal infections contribute to elevated systemic C-reactive protein level. J Periodontol 2001;72:1221-7.
5. Paraskevas S, Huizinga JD, Loos BG. A systematic review and meta-analyses on C reactive protein in relation to periodontitis. J Clin Periodontol 2008;35:277-90.
6. Tonetti MS, D'Aiuto F, Nibali L, et al. Treatment of periodontitis and endothelial function. N Engl J Med 2007;356:911-20.
7. Figuero E, Sanchez-Beltran M, Cuesta-Frechoso S, et al. Detection of periodontal bacteria in atheromatous plaque by nested polymerase chain reaction. J Periodontol 2011;82:1469-77.
8. Offenbacher S, Beck JD, Moss K, et al. Results from the Periodontitis and Vascular Events (PAVE) Study: a pilot multicentered, randomized, controlled trial to study effects of periodontal therapy in a secondary prevention model of cardiovascular disease. Journal of periodontology 2009;80:190-201.
9. Fifer KM, Qadir S, Subramanian S, et al. Positron emission tomography measurement of periodontal (18)f-fluorodeoxyglucose uptake is associated with histologically determined carotid plaque inflammation. J Am Coll Cardiol 2011;57:971-6.
10. Kito S, Koga H, Kodama M, et al. Reflection of (18)F-FDG accumulation in the evaluation of the extent of periapical or periodontal inflammation. Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:e62-9.
11.Cunha-Cruz J, Saver B, Maupome G, Hujoel PP. Statin use and tooth loss in chronic periodontitis patients. J Periodontol 2006;77:1061-6.
12. Saver BG, Hujoel PP, Cunha-Cruz J, Maupome G. Are statins associated with decreased tooth loss in chronic periodontitis? J Clin Periodontol 2007;34:214-9.
13. Meisel P, Kohlmann T, Wallaschofski H, et al. Cholesterol, CReactive Protein, and Periodontitis: HMG-CoA-Reductase Inhibitors (Statins) as Effect Modifiers. ISRN Dent 2011;2011:125168.
14. Lindy O, Suomalainen K, Makela M, Lindy S. Statin use is associated with fewer periodontal lesions: A retrospective study. BMC Oral Health 2008;8:16.
15. Fajardo ME, Rocha ML, Sanchez-Marin FJ, et al. Effect of atorvastatin on chronic periodontitis: a randomized pilot study. J Clin Periodontol 2010;37:1016-22.
