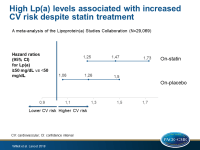
High Lp(a) levels associated with increased CV risk despite statin treatment
Meta-analysis of individual-patient data shows that elevated Lp(a) levels of 50 mg/dL or higher were associated with an increased hazard ratio of CV events, independent of other risk factors and statin or placebo treatment.
Baseline and on-statin treatment lipoprotein(a) levels for prediction of cardiovascular events: individual patient-data meta-analysis of statin outcome trialsLiterature - Willeit P, Ridker PM, Nestel PJ et al. - The Lancet 2018; published online ahead of print
Introduction and methods
Existing data show that elevated lipoprotein(a) (Lp[a]) levels are associated with increased risk of CHD, stroke, peripheral arterial disease, and calcific aortic valve stenosis [1-3]. However, the contribution of high Lp(a) levels to CV events in patients with established CVD with or without statin therapy is unclear.
This meta-analysis of the Lipoprotein(a) Studies Collaboration used 7 randomized, placebo-controlled trials [4-10] of statins with individual patient-level data for CVD outcomes and Lp(a) measurements at baseline and follow-up (under statin treatment), and evaluated the associations of baseline and on-treatment Lp(a) levels with CV risk.
In each study, CV outcomes, including fatal or non-fatal CHD, stroke, or revascularization procedures, were stratified by predefined Lp(a) groups (15 to<30 mg/dL, 30 to <50 mg/dL, and ≥50 mg/dL, vs <15 mg/dL).
Main results
- Out of a total of 45,044 patients, 35% were excluded because of missing Lp(a) measurements, leaving a sample of 29,069 patients for analysis, out of whom 14,536 patients were randomly allocated to statin treatment.
- The effect of statin treatment on Lp(a) concentration was heterogeneous across trials. The pooled percentage change was –0.4% (95%CI: –7 to 7), with 3 trials showing a mean increase (between 2% and 15%) and 4 trials showing a mean decrease (between –1% and –13%) in Lp(a) levels.
- The age- and gender-adjusted correlations between baseline and follow-up Lp(a) were comparable in patients receiving statin treatment and in those of the placebo group (r=0.948 vs r=0.952).
- The incidence of CV events per 1,000 person-years was 55.3 (95%CI: 53.4-57.3) in those with baseline Lp(a) <15 mg/dL, 56.3 (95%CI: 52.6–60.2) in those with Lp(a) levels between 15-<30 mg/dL, 66.7 (95%CI: 62.0–71.8) in those with Lp(a) levels between 30-<50 mg/dL, and 80.0 (95%CI: 75.3–84.9) in those with Lp(a) ≥50 mg/dL.
- Among patients receiving statin therapy, the incidence of CV events per 1,000 person-years was 49.0 (95%CI: 46.5–51.6) for Lp(a) <15 mg/dL, 46.4 (95%CI: 41.6–51.7) for Lp(a) 15-<30 mg/dL, 56.2 (95%CI: 50.3–62.8) for Lp(a) 30-<50 mg/dL, and 77.2 (95%CI: 71.1–83.8) for Lp(a) ≥50 mg/dL.
- These results remained similar after additional adjustment for previous CVD, diabetes, smoking, systolic blood pressure, and lipid levels.
- After multivariable adjustment, the HRs for CV events were 1.47 (95%CI: 1.25-1.73) for patients with Lp(a) ≥50 mg/dL treated with statins, and 1.26 (95%CI: 1.06-1.50) for patients receiving placebo (P-interaction =0.031), compared with patients showing Lp(a) levels lower than 50 mg/dL during a median follow-up of one year.
Conclusion
Elevated Lp(a) levels of 50 mg/dL or higher, at baseline or on-treatment, were associated with an increased risk of CV events, independent of other CV risk factors. The effect was evident on treatment with either statin or placebo. These data suggest existence of a residual risk in patients with elevated Lp(a) that is not addressed by statins and support the rationale for outcomes trials to test specific therapies to lower Lp(a).
References
1. Tsimikas S. A test in context: lipoprotein(a): diagnosis, prognosis, controversies, and emerging therapies. J Am Coll Cardiol 2017;69: 692–711.
2. Tsimikas S, Fazio S, Ferdinand KC, et al. NHLBI Working Group recommendations to reduce lipoprotein(a)-mediated risk of cardiovascular disease and aortic stenosis. J Am Coll Cardiol 2018;71: 177–92.
3. Thanassoulis G, Campbell CY, Owens DS, et al. Genetic associations with valvular calcification and aortic stenosis. N Engl J Med 2013;368: 503–12
4. Khera AV, Everett BM, Caulfield MP, et al. Lipoprotein(a) concentrations, rosuvastatin therapy, and residual vascular risk: an analysis from the JUPITER Trial (Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin). Circulation 2014; 129: 635–42.
5. Downs JR, Clearfield M, Weis S, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. JAMA 1998; 279: 1615–22.
6. Deshmukh HA, Colhoun HM, Johnson T, et al. Genome-wide association study of genetic determinants of LDL-c response to atorvastatin therapy: importance of Lp(a). J Lipid Res 2012; 53: 1000–11.
7. Kollerits B, Drechsler C, Krane V, et al. Lipoprotein(a) concentrations, apolipoprotein(a) isoforms and clinical endpoints in haemodialysis patients with type 2 diabetes mellitus: results from the 4D Study. Nephrol Dial Transplant 2016; 31: 1901–08.
8. Nestel PJ, Barnes EH, Tonkin AM, et al. Plasma lipoprotein(a) concentration predicts future coronary and cardiovascular events in patients with stable coronary heart disease. Arterioscler Thromb Vasc Biol 2013; 33: 2902–08.
9. Tsimikas S, Witztum JL, Miller ER, et al. High-dose atorvastatin reduces total plasma levels of oxidized phospholipids and immune complexes present on apolipoprotein B-100 in patients with acute coronary syndromes in the MIRACL trial. Circulation 2004;110: 1406–12.
10. Berg K, Dahlen G, Christophersen B, et al. Lp(a) lipoprotein level predicts survival and major coronary events in the Scandinavian Simvastatin Survival Study. Clin Genet 1997; 52: 254–61.