High red meat consumption associated with higher risk of type 2 diabetes mellitus
Reducing red meat intake lowered T2DM risk. WJ Evans PhD argues in an invited commentary that the specific fatty acid content rather than the colour should be focussed on to reduce health risks.
Changes in Red Meat Consumption and Subsequent Risk of Type 2 Diabetes Mellitus - Three Cohorts of US Men and WomenLiterature - Pan A, Sun Q, Bernstein AM et al. - JAMA Intern Med. 2013;():1-8
Pan A, Sun Q, Bernstein AM et al.
JAMA Intern Med. 2013;():1-8. doi:10.1001/jamainternmed.2013.6633
Background
Consumption of red meat has consistently been related to an elevated risk of type 2 diabetes mellitus (T2DM) [1-3]. However, often limited follow-up information was implemented, thus ignoring that eating behaviour may change over time. It is relevant to evaluate whether changes in red meat consumption over time have consequences for the risk of developing T2DM.This study therefore analysed data from 3 Harvard cohort studies, to wit the Health Professionals Follow-up Study (HPFS), the Nurses’ Health Study (NHS) and the Nurses’ Health Study II (NHSII). Repeated measurements of red meat intake and other dietary components were conducted every 4 years. Data on lifestyle factors and medical history were also collected. Follow-up time was up to 20 years, allowing to investigate the association between dynamic changes in red meat intake and subsequent risk of T2DM.
Main results
- Compared to people whose intake remained relatively stable in each 4-year period, those who increased their red meat intake were at elevated risks ( P<0.001 in all 3 cohorts). Increasing red meat intake by more than 0.50 servings per day was associated with 48% increased risk in the subsequent 4 years (pooled HR: 1.48, 95%CI: 1.37-1.59).
- After correction for initial BMI and concurrent weight gain, the association between increasing red meat intake by 0.50 servings/day and T2DM risk was mildly attenuated (HR: 1.30, 95%CI: 1.21-1.41).
- A moderate increase (0.15-0.50 servings/day) in red meat intake was also associated with an increased risk of T2DM before (pooled HR: 1.21, 95%CI: 1.13-1.30) and after (HR: 1.15, 95%CI: 1.07-1.23) adjustment for initial BMI and weight gain.
- After a reduction of red meat intake, no decreased T2DM risk was found within a 4-year period. When red meat exposure was related to the risk of developing T2DM during the entire follow-up, a reduction of more than 0.50 servings/day was associated with a reduced risk (pooled HR: 0.86, 95%CI: 0.80-0.93, and HR: 0.90, 95%CI: 0.83-0.97 after correction for initial BMI and weight gain).
- A significant interaction was seen between initial BMI and changes in red meat intake, in relation to T2DM risk. In non-obese individuals, the increased T2DM risk of greater intake (>0.50 servings/day) of red meat was greater (HR: 1.65, 95%CI: 1.48-1.84) than in obese individuals (HR: 1.14, 95%CI: 1.02-1.27).
Conclusion
In 3 large prospective cohorts of US men and women, a positive association was seen between 4-year increases in red meat consumption and subsequent 4-year risk of T2DM, independent of initial red meat intake and changes in other lifestyle factors. Decreasing red meat intake was not associated with an acutely reduced risk, but it did however induce a prolonged reduction of T2DM risk. These data suggest that the effect is partly but not entirely mediated through obesity and weight gain.Editorial comment [4]
This study provides valuable information for those considering strategies to decrease the risk of developing T2DM. However, the designation of meat according to its ‘redness’ is not an adequate description of the category of meat examined. The colour of meat is determined by its myoglobin and, to a lesser extent, its haemoglobin content. Some parts of chicken have more myoglobin than pork, and cuts tuna have almost twice the myoglobin content than beef. The description of red meat as a food category may therefore be misleading and has little value. The saturated fatty acid (SFA) content may be a better description of the characteristics of the meat with the greatest effect on risk than the amount of oxygen-carrying proteins. Recent studies reporting that only the consumption of processed meat (rich in SFA and total fatty acids), not other types of meat, was associated with a greater risk of incident coronary heart disease, stroke and T2DM, point in that direction. Effects of dietary fats like palmitate and stearate on insulin resistance have been described. It is, however, extremely difficult to control for the effects of these dietary fatty acids in observational studies. Public health messages should focus on eating the right type of fats, rather than the right type of meat. And that may include cuts of red meat that are low in fat.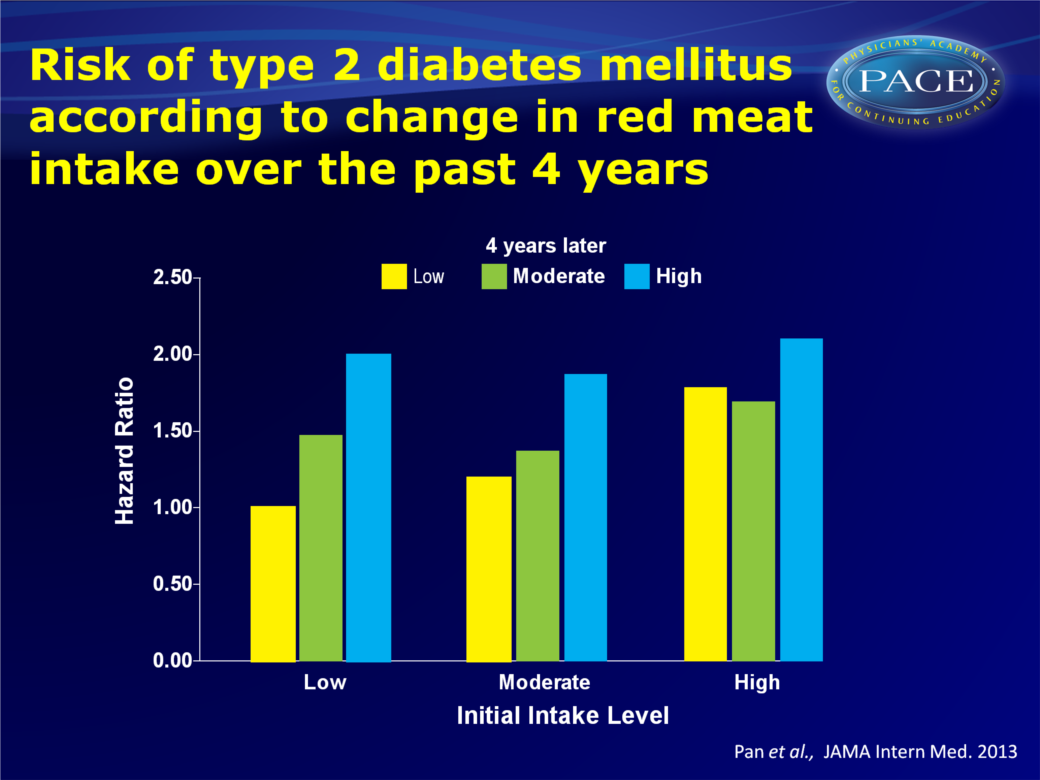
References
1. Aune D, Ursin G, Veierød MB. Meat consumption and the risk of type 2 diabetes: a systematic review and meta-analysis of cohort studies. Diabetologia. 2009; 52(11):2277-2287.
2. Micha R, Wallace SK, Mozaffarian D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation. 2010;121(21):2271-2283.
3. Pan A, Sun Q, Bernstein AM, et al. Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. Am J Clin Nutr. 2011;94(4):1088-1096.
4. Evans WJ. Oxygen-Carrying Proteins in Meat and Risk of Diabetes Mellitus. JAMA Intern Med. 2013;():1-2. doi:10.1001/jamainternmed.2013.7399
